Perinatal Asphyxia and the Associated Risk factors Among Neonates in Hayatabad Medical Complex, Peshawar
ABSTRACT
Introduction: Birth asphyxia is a common risk factor for many neonatal deaths worldwide. There can be multiple risk factors
due to which a neonate may not be able to take in enough oxygen before, during, or just after birth. This lack of oxygen can cause
serious damage to the brain tissues leading to complications like seizures and other neurological problems. This study aimed to
determine various perinatal risk factors associated with birth asphyxia in Hayatabad Medical Complex (HMC), Peshawar.
Methods: A cross-sectional study was carried out at the Neonatal Pediatric Department, Hayatabad Medical Complex, Peshawar
from June 2020 to December 2020. All neonates with birth asphyxia admitted to the neonatal intensive care unit (NICU) during
the study period with a low Apgar score of three or less at the first minute were enrolled. The socio-demographic information of
neonates and mothers was noted. A modified standard questionnaire was used. The data were analyzed through SPSS 22.
Results: A total of 145 newborns were enrolled. In cases, there were 99 males and 46 females. The majority of mothers [87
(60%)] were primiparous and 49 (33.8%) presented with anemia. Prolonged labor was noted in cases 29 (20%) while fetal distress
was found in 52 (35.9%) cases. Meconium was found in the amniotic fluid in 38 (26.2%) cases.
Conclusion: The major risk factors for birth asphyxia identified in our study were Meconium-stained liquor Prolonged and fetal
distress. Pakistan being still a developing country demands further research in this regard. On-time involvement of obstetricians,
proper education of the mother regarding care during pregnancy and awareness regarding the importance of antenatal screening
can be helpful in reducing the risk of birth asphyxia in neonates.
INTRODUCTION
Birth asphyxia is a lack of blood flow or gas exchange to or from the fetus in the period immediately before, during, or after the birth process [1]. A cell needs oxygen and nutrition to work properly Without this a cell cannot perform its functions normally. Lack of oxygen leads to accumulation of the waste products such as acids which build up in the cells and cause damage. This harm depends on (1) the level of oxygen (2) the duration the baby is deprived of oxygen (3) How timely the right treatment is given [2]. Multiple risk factors have been identified due to which a neonate may not be able to receive enough oxygen. It can be divided into three main causes i.e. a) Maternal problems, b) problems with the placenta and c) fetal problems such as the baby may not be able to breathe after delivery [3]. Birth asphyxia is the fifth largest cause of under-5 child deaths (8.5%), after pneumonia, diarrhea, neonatal infections and complications of pre-term birth and contributing to 23% of all newborn deaths [4].
Two-thirds of the world’s neonatal deaths occur in just 10 countries, mostly in Asia. Among these countries, Pakistan ranks third. With an estimated 298,000 newborn deaths annually and a reported neonatal mortality rate of 49 per 1,000 live births, Pakistan accounts for 7% of global neonatal deaths [5-7]. Various risk factors are associated with birth asphyxia such as meconium staining, prolonged rupture of membranes, maternal anemia, vaginal bleeding, mode of delivery etc. [8]. The American Academy of Pediatrics and a task force on cerebral Palsy have defined birth asphyxia as a persistently low Apgar score of 0-3 for ≥5 minutes along with neurologic manifestations due to asphyxia and multiorgan involvement e.g. cardiovascular, gastrointestinal, or renal compromise [9].
To find the contribution of birth asphyxia to the mortality and morbidity of neonates, detailed research needs to be done especially in the areas where the prevalence is higher due to unavailability’s of the proper facilities. Pakistan being a developing country still lacks research in this area and demands attention. In Peshawar, not much data is available on the prevalence of birth asphyxia along with the risk factors causing it. The findings of the present study can be utilized for policy making so that one can find the possible causes and plan to educate the public and create awareness regarding the risk factors, and hospital- based management strategies can be further strengthened and tailored. he main purpose of this study is to explore and address the gap in magnitude and associated factors of birth asphyxia.
MATERIALS & METHODS
The research was carried out at the Department of Pediatrics/ Neonatology HMC, Peshawar. Consent (written & informed) was taken from all mothers. The data was collected from June to December 2020 (six months). A total of 145 neonates were enrolled in the research. Neonates who were born in HMC and who fulfilled the definition of birth asphyxia were enrolled in the study. A detailed history was taken from the mother along with the examination of the neonates to look for any signs of birth asphyxia such as tone posture delayed cry etc. A modified standard questionnaire was used to collect data from the mothers of neonates with birth asphyxia and from medical records. The questionnaire comprises 26 questions in four sections. The demographic data of neonate and mother, maternal history, maternal history of current pregnancy, fetal conditions diagnosed during pregnancy, a maternal condition during labor and delivery, and neonatal characteristics. All the data were analyzed through SPSS version 22 for descriptive statistics. Association between birth asphyxia and risk factors was determined using the Chi-Square test.
RESULTS
The Demographic Data of Neonate and Mother
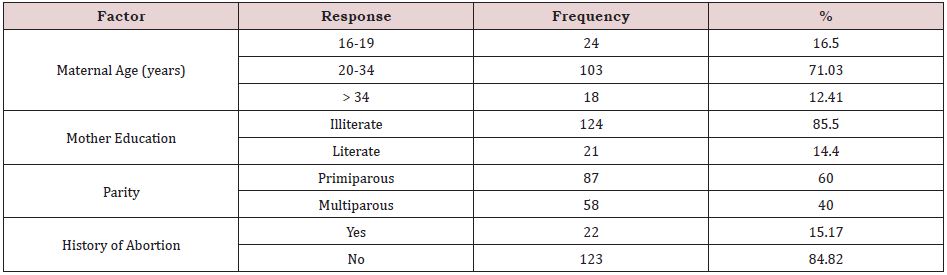
In this study, all 145 mothers approached agreed to participate, thus a response rate of 100 %. More than two-thirds of them (85.5%) were illiterate. The mean maternal age was 26.1 (SD = ±5.86) years of whom 71.03% were between 20 and 34 years (Table 1).
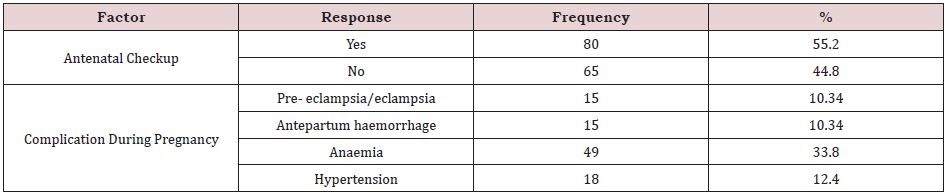
Eighty mothers [80(55.2%)] had attended antenatal care. In the antenatal period, obstetric complications were found in mothers. Of these complications, anemia accounted for the highest percentage 49 (33.8%); (Table 2).
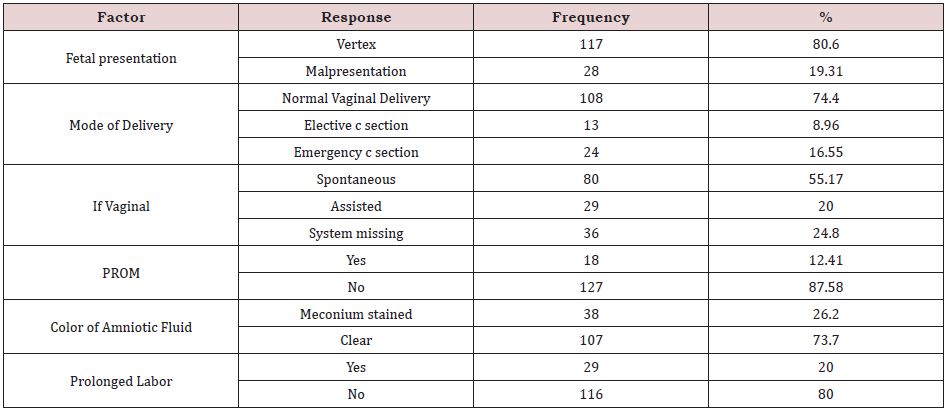
A maternal condition during labor and delivery, of the total respondent mothers, 108(74.5%) had normal vaginal delivery among which 80(55.2%) were delivered spontaneously. Premature rupture of the membrane was reported among only 18 (12.4%) mothers. Following membrane rupture, meconium-stained amniotic fluid was observed among 38 (26.2%) mothers at labor, about one-fifth of the fetuses 28(19.3%) were mispresented (Table 3).
Neonatal Characteristics
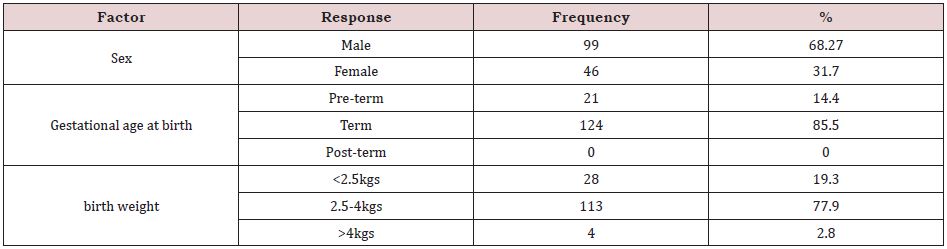
More than half of the newborns, 99(68.3%) were males. More than half of the newborns 124(85.5%) were term. Moreover, about one- fifth of the newborns 28(19.3%) had low birth weight (Table 4).
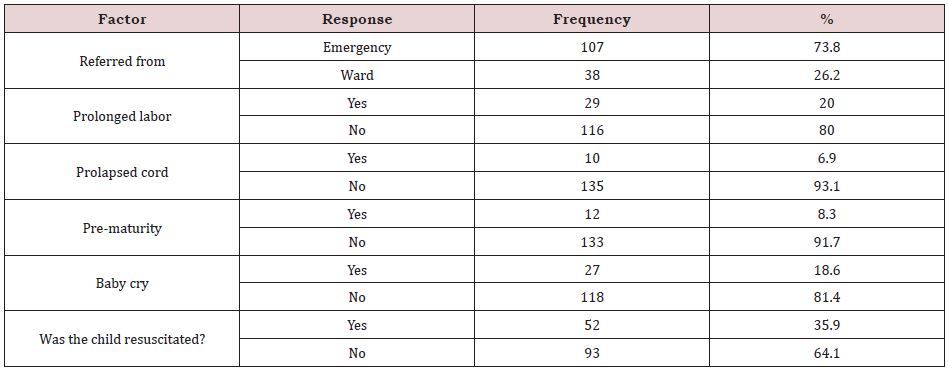
Around two-thirds [107 (73.8%)] were referred from the emergency department. A total of 29 (20%) only underwent prolonged labor whereas premature births were accountable for just 12(8.3%) of the newborns. Of the newborns with delayed birth cry were only 27 (18.6%); (Table 5).
DISCUSSION
This study was conducted to find the perinatal risk factors associated with birth asphyxia amongst the neonates born in Hayatabad Medical Complex, Peshawar, Pakistan. In the present study, male newborns were 68.3% as compared to females 31.7% which was 2:6:1male-to- female ratio in a study from the Children Hospital Lahore, Pakistan [10]. Our study showed multiple risk factors for birth asphyxia in which the leading cause was Primigravida (60%) This is in accordance with the studies conducted in India and Nepal [11,12]. The common reason is that during the first pregnancy the mother is usually not aware of her nutritional status and the importance of the antenatal checkups and the responsibilities towards the unborn fetus [13]. These reasons can contribute and can lead to fetal distress. In our study 35.9% of neonates born needed resuscitation, which is a significant number. Meconium-stained liquor was seen in only 26.4% of cases. This is an additional risk factor for fetal distress This is again in accordance with the studies done in the past [14- 20]. Prolonged labor was also observed as a significant risk factor for birth asphyxia This was similar to the studies conducted in the past in different parts of the world like Dhaka, Ethiopia, Nigeria, and Stockholm and Gotland Sweden [21-22]. some studies have shown an increase in birth asphyxia with an increase in gestational age which was similar in our study as well [23,24]. Our study also showed that birth asphyxia is more common between 20 and 34 years of age in the mother (71.03%) newborns were mostly delivered by normal vaginal delivery (74.5%) as compared to cesarean section particularly emergency c-section which in our case was 16.6%. Some studies found emergency cesarean section due to any reason to be an important risk factor for asphyxia [23]. Like every study, we too had limitations such as we were not able to record blood gases in diagnosing asphyxia due to unavailability of the adequate resources.
CONCLUSION
The major risk factors for birth asphyxia identified in our study were Meconium-stained liquor Prolonged and fetal distress. Pakistan being still a developing country demands further research in this regard. On-time involvement of obstetricians, proper education of the mother regarding care during pregnancy and awareness regarding the importance of antenatal screening can be helpful in reducing the risk of birth asphyxia in neonates.
REFERENCES
- Gillam-Krakauer M, Gowen CW (2019) Birth Asphyxia.
- Airway, Breathing and Lung Conditions: Birth Asphyxia (2019).
- Majeed R, Memon Y, Majeed F, Shaikh NP, Rajar UD (2007) Risk factors of birth asphyxia. J Ayub MedColl 19: 67-71.
- Farrar J, Hotez P, Junghanss T, Kang G, Lalloo D, et al. (2014) Paediatrics in the Tropics (Chapter 80) Manson’s Tropical Infectious Diseases 23rd Edn. China Elsevier.
- Lerberghe WV, Annick Manuel, Matthews Z, Cathy Wolfheim (2005) World health report 2005: Make every mother and child count. Geneva: WHO.
- Bhutta ZA, Hafeez A, Rizvi A Maternal and child health.
- Lawn JE, Cousens SN, Wilczynska K (2006) Estimating the causes of four million neonatal deaths in the year 2000: statistical annex. In The world health report 35(3): 706-18.
- Butt TK, Farooqui R, Khan MA (2008) Risk factors for hypoxicence phalopathy in children. J Coll Physicians Surg Pak 18(7): 428-32.
- Hankins GD, Speer M (2003) Defifining the pathogenesis and pathophysiology of neonatal encephalopathy and cerebral palsy. Obstet Gynecol 102: 628-36.
- Lahore Laeeq A, Iqbal MA, Maqbql S (2002) Risk factors analysis of birth asphyxia at children hospital Pak Pediatr J 26: 47-53.
- Gane B, Vishnu BB, Ramachandra R, Nandakumar S, Adhisivam B, et al. (2013) Antenatal and intrapartum risk factors for perinatal asphyxia: a case control study.
- Ellis M, Manandhar Z, Manandhar DS, Costello AM (2000) Risk factors for neonatal encephalopathy in Kathmandu, Nepal, a developing country: unmatched case-control study. 320(7244): 1229-1236.
- Adeoye S, Ogbonnaya LU. Umeorah OU, Asiegbu O (2005) Concurrent use of multiple antenatal care providers by women utilizing free antenatal care at Ebonyi State University Teaching Hospital, Abakaliki. Afr J Reprod Health 9(2):101-106.
- Gudayu TW (2017) Proportion and factors associated with low fifth minute Apgar score among singleton newborn babies in Gondar University referral hospital; Northwest Ethiopia. Afri Health Sci 17(1): 1-6.
- Sahib HS (2015) Risk factors of perinatal asphyxia: a study at Al Diwaniya maternity and children teaching hospital. Muthanna Med J 2(2): 50-57.
- Collins KA, Popek E (2018) Birth injury: birth asphyxia and birth trauma. Acad Forensic Pathol 8: 788-864.
- Onyearugha CN, Ugboma HA (2010) Severe birth asphyxia: Risk factors as seen in a tertiary institution in the Niger delta area of Nigeria. J Trop Med 4: 11-19.
- Chiabi A, Nguefack S, Evelyne M (2013) Risk factors for birth asphyxia in an urban health facility in Cameroon. Iran J Child Neurol 7: 46-54.
- Shireen N, Nahar N, Mollah A (2009) Risk factors and short-term outcome of birth asphyxiated babies in Dhaka Medical College Hospital. Bangladesh J Child Health 33(3): 83-89.
- Altman M, Sandström A, Petersson G, Frisell T, Cnattingius S, et al. (2015) Prolonged second stage of labor is associated with low Apgar score. Eur J Epidemiol. 30: 1209- 1215.
- Berhe YZ, Kebedom AG, Gebregziabher L (2020) Risk factors of birth asphyxia among neonates born in public hospitals of Tigray. Northern Ethiopia Pediatric Health Med Ther 11: 13-20.
- The investigation of rate of Birth Asphyxia and its relationship with delivery mode at Shahid Beheshti Hospital of Isfahan during. 23:10.
- Utomo MT (2011) Risk factors for birth asphyxia. Folia Medica Indonesiana 47: 211-214.
Article Type
Research Article
Publication history
Received Date: September 23, 2022
Published: November 01, 2022
Address for correspondence
Nouman Anthony, Rehman Medical institute Peshawar, Pakistan
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Nawal R, Sajjad A, Ahmad Ammar K, Syed Danial K, Anne G, Maaz K, Nouman A. Perinatal Asphyxia and the Associated Risk factors Among Neonates in Hayatabad Medical Complex, Peshawar. 2022- 4(6) OAJBS.ID.000508.