Neurological and Psychiatric Complications of SARSCOV- 2 in Children and Adults
ABSTRACT
Background: The pandemic has also resulted in the loss of livelihoods due to prolonged lockdowns, which have had a ripple
effect on the global economy. According to the World Health Organization, the emergence of viral diseases represents a serious risk
to public health. One of the mechanisms of action of this virus is through the ACE2 receptor. Different neurological findings caused
by COVID-19 have been described, among which we find anosmia, ageusia, headache, stroke, altered consciousness, among others,
as well as psychiatric symptoms.
Methodology: A systematic review was carried out through various databases; The search and selection of articles was carried
out in indexed journals in English.
Results: The exact route by which SARS-CoV-2 can enter the CNS is still unknown, although hypotheses have been raised, among
which we find the transsynaptic pathway, through the olfactory bulb, Regulation of ACE2-R and SIRS. Among the main psychiatric
symptoms found in the COVID-19 pandemic are symptoms of depression, anxiety symptoms, post-traumatic stress disorder
symptoms, and psychological distress. There is a relationship between the disturbance of the immune system and neuroinflammation
in the emergence of psychiatric diseases and high systemic inflammation in mood disorders, anxiety and psychotic disorders.
Conclusion: This review offers up-to-date and detailed information on the mechanisms of neurovirulence, the main neurological
complications, and neuropsychiatric mechanisms after SARS-COV-2 infection.
KEYWORDS
Complications; Neurological; Neuropsychiatric; SARS-COV-2; COVID-19
INTRODUCTION
Coronavirus disease 2019 (COVID-19), the highly contagious infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has had a catastrophic effect on global populations resulting in more than 6 million of deaths worldwide [1]. The pandemic has also resulted in the loss of livelihoods due to prolonged lockdowns, which have had a ripple effect on the global economy. Although substantial progress in clinical research has led to a better understanding of SARS-CoV-2 and the management of COVID-19, limiting the continued spread of this virus and its variants has become a matter of growing concern [2,3]. Despite the unprecedented speed of vaccine development against COVID-19 prevention and robust global mass vaccination efforts, including vaccine boosters, the emergence of new variants of SARS-CoV-2 threatens to reverse important progress. achieved so far to limit the spread of this viral disease [4]. According to the World Health Organization, the emergence of viral diseases represents a serious risk to public health. In the last two decades, several epidemics caused by viruses such as the severe acute respiratory syndrome coronavirus (SARS-CoV) from 2002 to 2003, and the H1N1 influenza in 2009, and the Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012 have been described as having a significant impact on global health [5,6]. One of the mechanisms of action of this virus is through the ACE2 receptor. There is emerging evidence of ACE2 receptors in human and mouse brains, implicating the possible infection of the brain by SARS-CoV-2. Possible routes by which SARS-CoV-2 can invade the central nervous system are transynaptic transfer across infected neurons via the olfactory nerve, infection of vascular endothelial cells, or leukocyte migration through the blood brain barrier [7,8].
In addition to anosmia and ageusia, other neurologic findings include headache, stroke, altered consciousness, seizure disorder, and toxic metabolic encephalopathy. Five patients with COVID-19 developed Guillain-Barré syndrome in a case series study [8-10]. In addition to the neurological effects that this disease could or may bring, the COVID-19 pandemic is also associated with very significant levels of psychological distress that, in many cases, would reach the threshold of clinical relevance. Mitigating the dangerous effects of COVID-19 on mental health is considered an international public health priority [11, 12]. The main psychiatric symptoms found in the COVID-19 pandemic are depression symptoms, anxiety symptoms, post-traumatic stress disorder symptoms, psychological distress. Timely dissemination of accurate and up-to-date COVID-19-related health information by authorities was shown to be associated with lower levels of anxiety, stress, and depressive symptoms in the general public [13]. Therefore, it is necessary to carry out this work in order to provide updated and accurate information on the mechanisms of neurovirulence, the main neurological complications and neuropsychiatric mechanisms after SARS-COV-2 infection.
MATERIALS AND METHODS
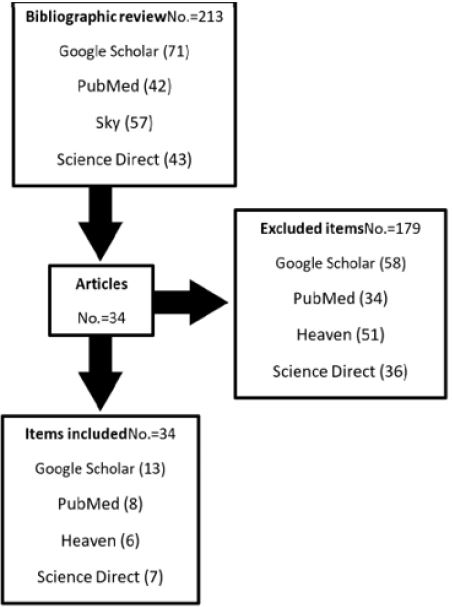
In this work we have carried out a systematic review, the databases that we implemented were PubMed, Scielo and ScienceDirect, among others. The English language was the main language on which our search was based, articles were collected from the year 2019 to the current date 2020. As keywords, the terms were used in the databases according to the DeCS and MeSH methodology: Complications; Neurological; Neuropsychiatric; SARS-COV-2; COVID-19. We have identified 213 original and review publications related to the subject studied, but only 34 articles met our inclusion criteria, such as articles that were in a range of no less than the year 2019, that were full-text articles and that reported on the theme. As exclusion criteria, it was taken into account that the articles did not have sufficient information and that they did not present the full text at the time of their review. In Figure 1, we can find a flowchart regarding the search.
RESULTS
Proposed Mechanisms of Sars-Cov-2 Neurovirulence
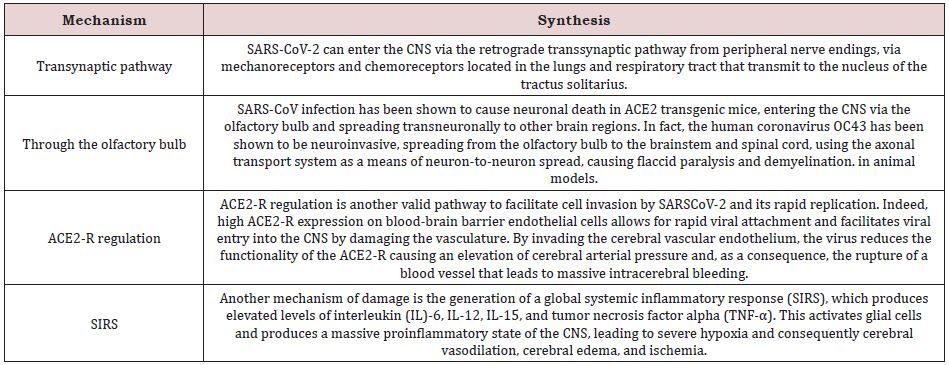
As has been studied and as is known, coronaviruses belong to a family of corona virus, which consists of four genera (alpha-, beta- , delta- and gamma-coronavirus) [14,15]. In order to develop this section correctly, we must ask ourselves the following question: How can Coronaviruses directly or indirectly affect the brain, developing neurological complications? To date, the vast majority of respiratory viruses have the ability to penetrate the central nervous system, causing the so-called neuro invasion, causing neurotropism (involvement of both neurons and glial cells) and thus causing various neurological pathologies (Neurovirulence) [16,17]. The exact route by which SARS-CoV-2 can penetrate the CNS is still unknown. Hypotheses have been raised. Table 1 shows the main proposed mechanisms [18-20].
Main Neurological Symptoms of Covid-19 Infection
One of the symptoms with the highest prevalence and incidence is headache. Apparently, this could be a symptom of little importance or relevance in some patients, but it has been shown that of the reported cases it was discovered that 15% of patients with this symptom had severe disease, 13.7% had elevated creatine levels kinase and in 0.2% of patients had rhabdomyolysis [21,22]. Smell and taste disorders may be the first neurological symptoms described in these patients. The underlying pathogenic mechanism that could explain the taste and smell disturbances in SARS-CoV-2 infection is a trans neural penetration through the olfactory bulb or penetration through the ACE-R [23]. Patients with more severe COVID-19 symptoms are likely to have other neurological symptoms, such as acute cerebrovascular disease, impaired consciousness, and skeletal muscle injury.
Acute Complications Associated with Covid 19
Meningoencephalitis
It is defined as inflammation of the meninges. The meninges are the three membranes (the dura mater, the arachnoid mater, and the pia mater) that line the vertebral canal and the skull that encloses the brain and spinal cord. Meningitis can have a varied clinical presentation depending on the age and immune status of the host. Symptoms often include fever, neck pain/stiffness, and photophobia. More nonspecific symptoms include headache, dizziness, confusion, delirium, irritability, and nausea/vomiting. Signs of increased intracranial pressure (altered mental status, neurological deficits, and seizures) portend a poor prognosis. The first reported case was described on March 4, 2020, at Ditan Hospital in Beijing. Subsequently, a second case was described in a 24-year-old Japanese man, with SARS-CoV-2 RNA detected only in cerebrospinal fluid (CSF) and hyperintense areas on MRI in the right lateral ventricle, the mesial region of the lobe. temporal and hippocampus. The pathophysiological mechanism of this pathology is still not completely clear, but it has been suggested that it could be caused in two ways, the first through edema secondary to the inflammatory lesion and the second through a direct viral infection of the CNS. Another case was recorded in Los Angeles, a young woman with COVID-19 showed symptoms of meningoencephalitis without respiratory failure, and CSF was found to be positive for SARS-CoV-2 by reverse transcription polymerase chain reaction (PCR); [23].
Acute disseminated encephalomyelitis
It is an acute and rapidly progressive autoimmune process characterized by demyelination of the brain and spinal cord as a result of inflammation. The case of a 40-year-old woman with diffuse hyperintensities in subcortical and deep white matter has been reported. Also, that of a 51-year-old woman who developed coma and impaired unilateral oculocephalic response weeks after a SARS-CoV-2 infection with radiological evidence of acute disseminated encephalomyelitis. In addition, autopsy of a 71-yearold patient diagnosed with COVID-19 showed scattered clusters of macrophages, axonal injury, and a perivascular acute disseminated encephalomyelitis-like appearance in the subcortical white matter [25].
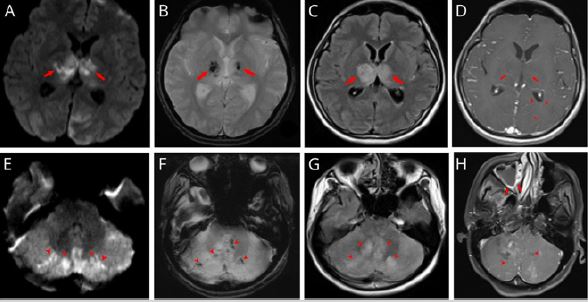
Acute necrotizing encephalopathy
Acute necrotizing encephalopathy is a rare but distinctive type of acute encephalopathy with a global distribution. The onset of acute necrotizing encephalopathy is usually preceded by a febrile illness associated with the virus and followed by rapid deterioration [26]. At present, the ethology and pathogenesis of acute necrotizing encephalopathy remain incompletely clear. Both environmental factors, which may contribute to preceding infections, and host factors, such as individual susceptibility or gene alterations, could be involved. Patients with acute necrotizing encephalopathy do not have specific symptoms or typical neurological signs. Comparisons of clinical features between Asian and non-Asian patients revealed the homogeneity of the disease throughout the world [27]. In addition to prodromal symptoms due to different viral infections, including fever, signs of upper respiratory tract infections, and gastroenteritis and erythema, patients with acute necrotizing encephalopathy often have signs of SIRS such as shock, multiple organ failure, and disseminated intravascular coagulation [28]. Acute Necrotizing Encephalopathy is a rare complication recently described in patients with COVID-19. The pathogenesis is related to cytokine release syndrome, a well-known manifestation of COVID-19. Typical MRI findings include hyperintense lesions and hemorrhage in the thalamus, brainstem, cerebellum, and cerebral white matter. Figure 2 shows the case of a 33-year-old woman who developed acute necrotizing encephalopathy and myocarditis in a previously healthy young patient with COVID-19 who was admitted due to generalized status epilepticus. Four days earlier she had developed generalized fatigue, fever, headache, and nasal congestion. On her arrival at the hospital she was comatose. She was emergency intubated and started on mechanical ventilation and received IV midazolam and valproic acid for seizure control. The CT scan of her head showed diffuse cerebral enema. On day 2, brain MRI showed bilateral haemorrhagic thalamic and cerebellar lesions [29]. On day 5 of his hospital stay, he suffered cardiopulmonary arrest and resuscitation attempts were unsuccessful. One day later, the results of her nasopharyngeal swab confirmed the detection of SARS-CoV2 by PCR.
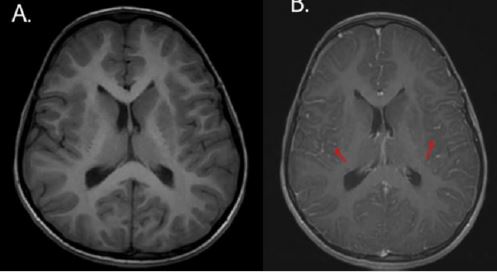
Epilepsy
One of the serious complications of COVID-19 is epileptic seizures. For critically ill patients with COVID-19, new-onset seizures should be considered acute symptomatic seizures. Studies have reported focal status epilepticus as the onset of COVID-19 in the setting of predisposing but well-controlled SARS-CoV-2- related postencephalitic epilepsy. Janardhan report on the case of a 6-year-old boy, who presented with focal seizures without a history of epilepsy. The child had twitching movements on the right side of the face involving the oral cavity. Noncontract brain MRI showed meningoencephalitis, Figure 3. He received antibiotics, antipyretics, and antiepileptic drugs, but his clinical condition continued to deteriorate despite treatment. Oropharyngeal and nasopharyngeal swabs were positive for COVID-19. Thus, treatment for encephalitis and seizures due to COVID-19 was started with intravenous immunoglobulin and steroids. Seizure frequency decreased dramatically after steroids were started and remained infrequent through five days of steroid therapy. After stopping the steroids, the seizures returned, but they were shorter, less frequent, and manageable with antiepileptic drugs.
Subacute Complications Associated with Covid 19
Myelitis
Transverse myelitis is a rare acquired focal inflammatory disorder that often presents with rapid-onset weakness, sensory deficits, and bowel/bladder dysfunction. This pathology usually occurs in the spinal cord at any level, but more commonly affects the thoracic region. The disorder traverses the spinal cord, causing bilateral deficiencies. However, there can only be partial or asymmetric involvement. The duration of this disease can be as short as 3 to 6 months or it can be permanently debilitating. At maximum deficit, 50% of patients are complete paraplegics and virtually all patients have some degree of bladder/bowel dysfunction. To date, several cases of acute transverse myelitis following COVID-19 infection have been reported. A study carried out by Chow reported on a 66-year-old man who presented acute flaccid paralysis of the bilateral lower limbs and urinary and intestinal incontinence due to multifocal transverse myelitis after COVID-19 infection. Similar to another study by the report on a 69-year-old woman who was diagnosed with acute necrotizing myelitis based on clinical symptoms and MRI findings.
Psychiatric Complications Associated with Covid 19
One of the most complex approaches and with potentially devastating consequences both for the individual and for the society or community that surrounds them, are the mental disorders that this disease, COVID-19, entails. Different studies have shown that patients with COVID-19 exhibited higher levels of depression, anxiety, and PTSD symptoms, with these three being the most prevalent [30].
Neuropsychiatric Mechanisms After Covid-19 Infection
To date these mechanisms are not entirely clear, further studies are still needed to be able to clearly identify these psychological processes after SARS-COV-2 infection. But some mechanisms have been suggested that could be involved or associated with the development of neuropsychiatric disorders or sequelae.
a) Somatic symptoms and medical care
b) Immune response
c) neurocognitive effects
d) Psychosocial conditions.
Social isolation and uncertainty about the future can induce or worsen post-infection neuropsychiatric conditions. However, the biological links between SARS-CoV-2 and mental health should not be ignored: direct neuronal injury to the central nervous system, immunoinflammatory activation that induces thrombosis and vascular damage, and its residue after recovery, could have key implications for these psychiatric disorders. One of the main causes of cognitive and psychological deterioration is present in those patients who required mechanical ventilation, approximately 80% of patients who survive acute respiratory failure after receiving mechanical ventilation develop post-intensive care syndrome. One study reported that approximately 40 to 88% of severe COVID-19 patients had neurological symptoms, associated with neuroinflammation, demyelination, and neurodegeneration, such as acute cerebrovascular disease or impaired consciousness [31].
Cytokine Storm and Psychiatric Complications
SARS-COV-2 infection can cause the so-called “cytokine storm”, that is, the local and systemic production of cytokines, chemokines and other inflammatory mediators. Studies show that SARS-CoV-2 induces high levels of interleukin (IL)-1β, IL-6, interferon (IFN)-γ, CXCL10, CCL2, and cytokines secreted by T-helper-2 cells such as IL-4 and IL-10.These highly expressed cytokines can have a variety of side effects, including disruption of the hypothalamicpituitary- adrenal and neuroendocrine axes, further compromising host immunocompetence. Many studies have pointed to the role of immune system perturbation and neuroinflammation in the emergence of psychiatric illnesses and of high systemic inflammation in mood, anxiety, and psychotic disorders.
DISCUSSION
The past two decades have been marked by three epidemics linked to emerging coronaviruses, severe acute respiratory syndrome (SARS) in 2002, Middle East Respiratory Syndrome (MERS) in 2012, and the ongoing coronavirus disease 2019 (COVID) pandemic-19. Other human coronaviruses (HCoV) circulate ubiquitously and are responsible for mild infections of the upper or lower respiratory tract. The first cases of COVID-19, the disease related to SARS-CoV-2, were reported in China in December 2019. Since then, the virus has continued to spread and as of March 11, 2020, the World Health Organization (WHO) characterized COVID-19 as a pandemic. This pandemic has brought many adverse effects, both for the country’s economy and health, emphasizing in this work the neurological and psychiatric manifestations. In the systematic review conducted by Maury et al. [32] they found 5 cohorts that provided data on the prevalence of neurological symptoms among a total of 2533 hospitalized patients with COVID-19 and articles focused on patients with COVID-19 with neurological manifestations that included a total of 580 patients. Concluding to confirm many manifestations and neurological diseases associated with SARS-CoV-2, including many pathogenic pathways that include infectious mechanisms, septic-associated encephalopathies, coagulopathy or enthesitis, although they do not affirm the direct pathogenicity of SARS-CoV-2.
Psychiatric manifestations are not only prevalent in adults, but also in adolescents. The study carried out by Benjamín et al. [33] in their systematic review of the literature, confirms that prolonged confinement at home, brutal mourning, violence family, excessive use of the Internet and social networks are factors that can influence the mental health of adolescents. Thus, increasing psychiatric disorders, such as post-traumatic stress, depression and anxiety disorders, as well as symptoms related to grief. As confirmed by the study carried out by Angelina et al. [34] in their cross-sectional study, of 2018 adolescent between April 22 and 28, 2020, in which half of the adolescents experienced anguish in the pandemic. Although the COVID-19 pandemic is no longer in force and the confinement has ended in recent months, it is necessary to study these facts in more depth to be prepared for future diseases that cause mass confinements.
While these and many other studies confirm the neurological and neuropsychiatric findings caused by COVID-19. A strength of the current study is the methodology implemented, regarding the literature search, and steps in the selection of relevant articles, quality assessment, and data extraction. However, this study has several limitations, which should be taken into account before reaching a conclusion, among these are the lack of clinical trial analysis studies regarding management, therapeutic approaches, and care protocols to provide a proper care in the prevention and management of neurological and psychiatric manifestations, so more studies are needed to answer these questions.
CONCLUSION
The exact route by which SARS-CoV-2 can enter the CNS is still unknown, although hypotheses have been raised, among which we find the transsynaptic pathway, Through the olfactory bulb, Regulation of ACE2-R and SIRS . One of the symptoms with the highest prevalence and incidence is headache, just as smell and taste disorders may be the first neurological symptoms described in these patients. Among the acute complications we find Meningoencephalitis, Acute Disseminated Encephalomyelitis, Acute Necrotizing Encephalopathy and Epilepsy. And of the subacute complications we find myelitis. Among the main psychiatric symptoms found in the COVID-19 pandemic are symptoms of depression, anxiety symptoms, post-traumatic stress disorder symptoms, and psychological distress. Although the COVID-19 pandemic is no longer in force and the confinement has ended in recent months, it is necessary to study these facts in more depth to be prepared for future diseases that cause Re-confinement.
REFERENCES
- Wang Y, Di Y, Ye J, Wei W (2020) Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 1-10.
- Wang C, Pan R, Wan X, Tan Y, Xu L, et al. (2020) A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 87: 40-48.
- Thakur V, Jain A (2020) COVID 2019-Suicides: a global psychological pandemic. Brain Behav Immun 88: 952-953.
- Sawalha AH, Zhao M, Coit P, Lu Q (2020) Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. J Clin Immunol 215: 108410.
- Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N (2020) Stress, anxiety and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude 36(4).
- McIntyre RS, Lee Y (2020) Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res 290: 113104.
- Li Z (2020) Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immum 88: 916-919.
- Guo W, Li M, Dong Y, Zhou H, Zhang Z, et al. (2020) Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab 36(7).
- Eid RS, Gobinath AR, Galea LAM (2019) Sex differences in depression: insights from clinical and preclinical studies. Prog Neurobiol 176: 86- 102.
- Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, et al. (2020) C4591001 Clinical Trial Group. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med 383(27).
- (2021) Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7. bioRxiv 593(7857): 130-135
- Joyner MJ, Senefeld JW, Klassen SA, Mills JR, Johnson PW, et al. (2021) Effect of Convalescent Plasma on Mortality among Hospitalized Patients with COVID-19: Initial Three-Month Experience. medRxiv
- Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, et al. (2020) Neuropathological Features of Covid-19. N Engl J Med 383(10): 989-992.
- Romano SD, Blackstock AJ, Taylor EV, El Burai Felix S, Adjei S, et al. (2020) Trends in Racial and Ethnic Disparities in COVID-19 Hospitalizations, by Region - United States, March-December 2020. MMWR Morb Mortal Wkly Rep 70(15): 560-565.
- Wibmer CK, Ayres F, Hermanus T, Madzivhandila M, Kgagudi P, et al. (2021) SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. Nat Med 27(4): 622-625.
- Chan JF, Kok KH, Zhu Z, Chu H, To KK, et al. (2020) Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect 9(1): 221-236.
- Raciti L, Calabrò RS (2020) Can volcanic trace elements facilitate Covid-19 diffusion? A hypothesis stemming from the Mount Etna area, Sicily. Med Hypotheses 144: 110058
- Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, et al. (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382(16): 1564-1567.
- Fu L, Wang B, Yuan T (2020) Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and metaanalysis. N Engl J Med 382(18): 1708-1720.
- Zhou F, Yu T, Du R (2020) Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229): 1054-1062.
- Gutiérrez-Ortiz C, Méndez A, Rodrigo-Rey S, San Pedro-Murillo E, Bermejo-Guerrero L, Gordo-Mañas R (2020) Miller Fisher Syndrome and polyneuritis cranialis in COVID-19. Neurology 95(5): e601-e605.
- Juliao Caamaño DS, Alonso Beato R (2020) Facial diplegia, a possible atypical variant of Guillain-Barré Syndrome as a rare neurological complication of SARS-CoV-2. J Clin Neurosci 77: 230-232.
- Paybast S, Gorji R, Mavandadi S (2020) Guillain-Barré Syndrome as a Neurological Complication of Novel COVID-19 Infection: A Case Report and Review of the Literature. Neurologist (4):101-103.
- Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, et al. (2020) Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol 77(8): 1018-1027.
- Madia F, Merico B, Primiano G, Cutuli S, De Pascale G, Servidei S (2020) Acute myopathic quadriplegia in COVID-19 patients in the intensive care unit. Neurology 95(11): 492-494.
- Joseph SJ, Gonçalves AP, Paul A, Bhandari SS (2020) Theoretical orientation of a range of psychological approaches to address mental health concerns during the COVID-19 pandemic. Asian J sychiatry 53: 102221.
- Hoertel N, Sánchez-Rico M, Vernet R, Beeker N, Jannot AS, Neuraz A, et al. (2021) Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Mol Psychiatry 26(9): 5199-5212.
- Carvalho PM, de M, Moreira MM, de Oliveira MNA, Landim JMM, et al. (2020) The psychiatric impact of the novel coronavirus outbreak. Psychiatry Res 286: 112902.
- Pallanti S, Grassi E, Makris N, Gasic GP, Hollander E (2020) Neurocovid-19: a clinical neuroscience-based approach to reduce SARS-CoV-2 related mental health sequelae. J Psychiatr Res 130: 215-217.
- Taquet M, Luciano S, Geddes JR, Harrison PJ (2020) Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 8(2): 130-140.
- Troyer EA, Kohn JN, Hong S (2020) Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun 87: 34-39.
- Maury A, Lyoubi A, Peiffer N, Broucker T, Meppiel E (2021) Neurological manifestations associated with SARS-CoV-2 and other coronaviruses: A narrative review for clinicians. Rev Neurol (Paris) 177(1-2): 51-64.
- Benjamin S, Lachal J, Radjack R, Carretier E, Minassian S, et al. (2020) Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res 291: 113264.
- Angelina S, Kurniawan A, Handy F, Adella D, Wijovi F (2021) Adolescents’ mental health status and influential factors amid the Coronavirus Disease pandemic. Clin Epidemiol Glob Health 12: 100903.
Article Type
Research Article
Publication history
Received Date: December 06, 2022
Published: February 21, 2023
Address for correspondence
Yaneth del Carmen Ramírez Quiñones, Psychiatry Resident, Universidad de Ciencias Médicas de La Habana, Cuba
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Yaneth del Carmen RQ, Blanca nieves SS, Adela Esperanza MC, Diana Carolina OC, et. al. Neurological and Psychiatric Complications of SARS-COV-2 in Children and Adults. 2023- 5(1) OAJBS.ID.000548.
Figure 1: Flowchart of the methodology implemented in this work.
Figure 2: Acute necrotizing encephalopathy and myocarditis in a young patient with COVID-19.
Figure 3: Magnetic resonance imaging of the brain that showed meningoencephalitis in a six-year-old boy.
Table 1: Main mechanisms of neuropathogenicity by SARS-COV-2.