Association Between Covid-19 Disease and Mortality After Hip Fracture Surgery in Elderly: A Multicentre National French Survey
ABSTRACT
Background: Although Covid-19 and major surgery have been linked to mortality, controversy exists about the risk of higher
mortality in the context of hip fracture. The objective of this study was to assess the association between mortality (30th day
postoperatively) and hip fracture surgery in patients with Covid (PCR+ 30 days) before surgery.
Methods: This was a population-based, retrospective cohort study of adults undergoing hip fracture surgery between March
1st and December 31st, 2020, at private or public hospitals in France. Patients were adults, > 65 yrs, with hip fracture admitted for
surgery. SARS-Cov2 infection within 30 days before surgery was recorded. Main outcome was mortality within 30 days after surgery.
Secondary outcomes included univariate and multivariate analysis of the association between subject characteristics and death at
30 days.
Results: Among 73.661 patients with hip fracture (mean age 85+ or -7.9 yrs, 76% women) who met study entry criteria, overall
mortality at 30 days was 4.8%. Among them, mortality in non-Covid patient was recorded for 3.304 (4.58%). For patients with
SARS-Cov2 infection (1.505 patients), mortality was recorded for 228 (15.15%; p(Khi-2) <.0001. The pair hip fracture and Covid-19
were associated with higher risk of mortality: OR, 3.72; 95%CI, 3.21-4.30; P< 00.1.
Conclusion: Among adults undergoing hip fracture surgery, Covid-19 infection was associated with a greater risk of 30-day
mortality.
KEYWORDS
Hip fracture; Covid-19; Mortality; Surgery; Elderly
INTRODUCTION
Hip fracture in the elderly is a worldwide public health issue and a medical challenge for early postoperative rehabilitation [1]. More than 2 million people are treated annually with an annual incidence between 100 and 300/100.000 (USA, Europe, China), resulting in a cost of billion dollars and a strain on most surgical facilities [2,3]. In this context, an early surgical management of patient with fracture within the first 24-48h has been shown to reduce morbidity, length of hospital stays and mortality (at 30 days: 5-10 %); [4].
During the Covid-19 pandemics, a higher risk of 30-day mortality has been reported in patients with pre-operative SARSCoV- 2 infection diagnosed from 0 to 6 weeks before surgery compared with patients who did not have a pre-operative SARSCoV- 2 infection [5, 6]. However, this risk seems to disappear in patients diagnosed with SARS-CoV-2 ≥ 7 weeks before surgery [6]. These findings led to propose delayed elective surgery when the benefit-risk ratio was acceptable (cancer, cardiac surgeries); [6,7]. However, delaying surgery in COVID-19 patients (with high risk of immune and thrombotic disorders) with hip fracture could be questionable as the risk related to COVID-19 could be counteracted by the risk delayed surgery.
Recently, several brief report and meta- analysis highlighted higher risk of mortality after hip fracture associated with SARSCoV- 2 infection [8,9]. For assessing the mortality risk related to hip fracture surgery associated with COVID-19 on large cohort over first and second wave, we used the French national hospital discharge records database for comparing the 30-day postoperative mortality in patients with hip fracture and with or without a hospitalization for SARS-COV-2 infection in the 30 previous days before surgery [6].
METHODS
Study Design and Data Source
The present study used data from the French national hospital discharge records database (resulting from the “French Prospective Payment System”, I), which systematically collects administrative and medical information related to all patients hospitalised and all hospital stays in private and public hospitals [10]. It is routinely completed for the purpose of care reimbursement, supporting its suitable accuracy and exhaustive data collection. The available data are age, gender, entry and discharge dates, diagnoses’ codes associated to the hospitalizations (according to international classification of diseases (ICD, Tenth Revision, Clinical Modification (ICD-10-CM)), death during a hospitalization. Concerning patients and stays, data are entered by physician daily and/or when the patient is discharged The French Ministry of Health (Assurance Maladie) regularly controls the quality of the database. The researchers and health institutions who collect their data according to the current guidelines could access to the complete database [10]. The retrospective design of prospectively and anonymously collected data was approved by the Institutional Review Board of the University Hospital Caremeau, Nimes, France (IRB 2021.05.21: 21.0034) and registered on Clinical Trials (NCT NCT04944329). According to the French current law, no informed consent was required [11]. STROBE recommendations for observational studies were followed.
Patients with Hip Fracture, and With or Without a SARSCOV- 2 Disease
We included patients ≥ 65-year-old with hip fracture hospitalization recorded between March 1st and December 31st 2020, detected through ICD-10 diagnosis codes that begin with femoral neck fracture, trochanter fracture or subtrochanteric fracture, and with a DRG Codes (Diagnosis Related Group) code indicating a surgical procedure (hip protheses for recent trauma, hip, and femur surgery for recent trauma). Patient with hip fracture hospitalization without a care code indicating a surgical procedure were excluded.
In these patients, we searched for hospitalizations with SARSCoV2 diagnostic that occurred within 30 days before the date of hospital admission for hip fracture. For this we used the following codes: COVID-19 respiratory form identified virus, COVID-19 respiratory form unidentified virus, COVID-19 carrier of SARSCoV- 2 asymptomatic identified virus, COVID-19 other clinical forms identified virus, COVID-19 other clinical forms unidentified virus. Patients with only a code “Other examinations and observations related to the epidemic COVID-19” were not retained as positive for SARS-COv2 disease.
Primary endpoint: The primary end point was in-hospital mortality within 30 days of the date of hospital admission for hip fracture. This criterion is collected exhaustively in the French national hospital database.
Secondary endpoint: Secondary outcomes included univariate and multivariate analyses of the association between subject characteristics and death at 30 days
Statistical Analysis
The patient characteristics are described with absolute numbers and proportions for categorical variables and with means and standard deviations (SD) for quantitative variables. Comparisons between groups were performed using Wilcoxon test for quantitative variables and the Chi-square for qualitative variables. To analyse the effect of SARS-Cov2 infection on 30-day postoperative mortality independently of potential confounders, we performed univariate and multivariate logistic regression models. The results are presented with odds ratios and their 95% confidence intervals. Interactions between SARS-COV2 infection and other available variables were all tested in successive multivariate logistics models. All analyses were conducted by the medical statistics department of the Nimes University Hospital using SAS software (V.9.4, SAS Institute, Cary, NC, USA). A two-sided p-value of <0.05 was considered to indicate statistical significance.
RESULTS
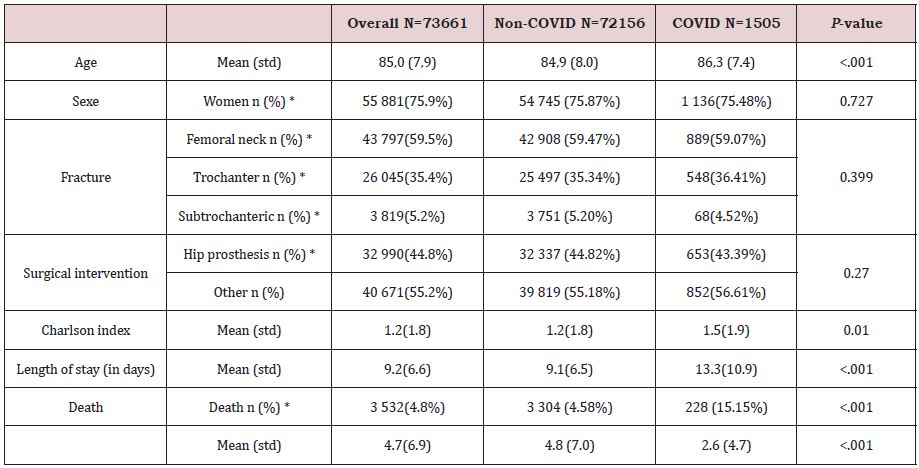
During the study period, 73.661 patients underwent a hip fracture surgery in France (Table 1) and a SARS-COV2 infection was diagnosed within 30 days before surgery in 1.505 (2.04%) patients of them. Table 1 shows patients characteristics according to COVID and Non-COVID status. Patients with COVID were older, with a higher Charlson comorbidity Index score and had a longer length of stay in hospital. The geographical location of traumatic fall (at home: 93% for Non Covid vs 88% for Covid), Fracture location and type of surgical interventions and time for surgery were similar. In 1505 COVID patients (2.04%), the SARS-COV2 infection was diagnosed during the Hip fracture hospitalization. The mean time from hospitalization with a diagnosis of SARS-COV2 to hospitalization for hip fracture was 1.73 (SD:5.77) days.
Primary Outcome
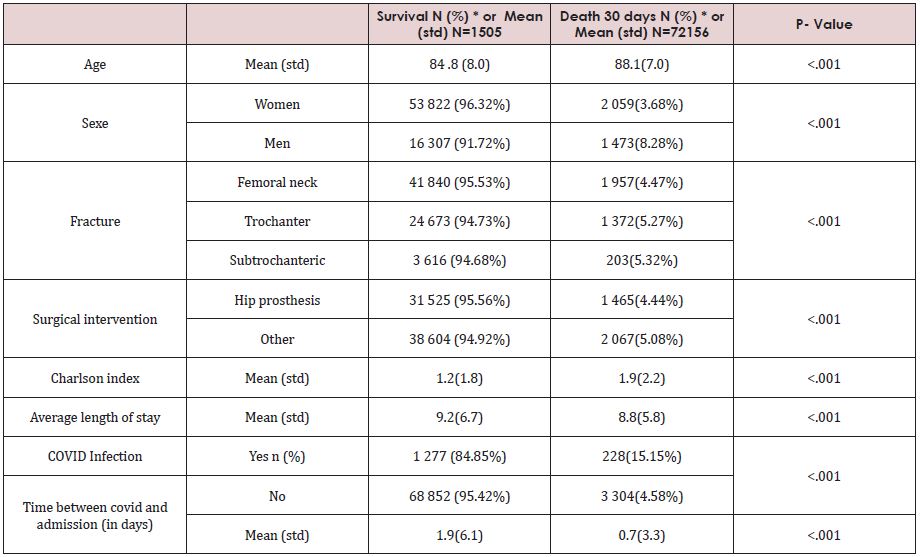
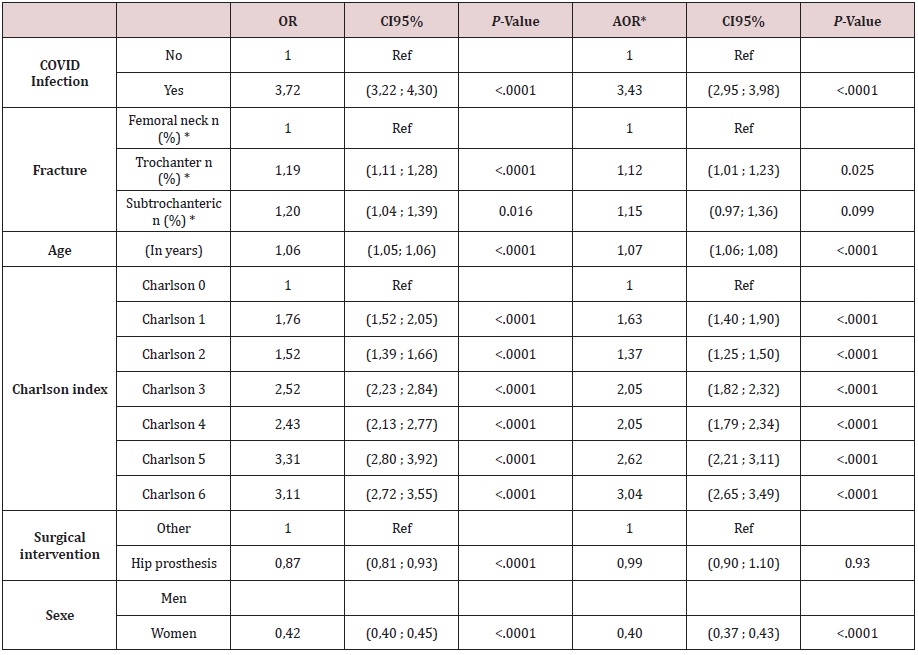
In patients with hip fracture, 3532/73,661 patients (4.8%) died in the first 30-day postoperative days. The 30-day postoperative mortality was significantly higher in patients with SARS-Cov2 infection (228/1505 (15.15%) vs 3305/72156 (4.58%), p-value <0.001, crude OR: 3.72, 95%CI [3.21-4.30]). After adjustment for age, sex, Charlson comorbidity Index score, fracture location, and type of surgery, the SARS-COV-2 infection within the 30 preoperative days was associated with a higher mortality rate (adjusted OR: 3.42 95%CI:2.94-3.97). Table 2,3 show the factors associated with a higher mortality rate. In multivariate analyses age, sex, Charlson comorbidity Index score, fracture location, and type of surgery were independently associated with 30-day postoperative mortality (Table 3). No effect statistical interaction of SARS-COV2 infection with other variables available (notably age) was found to be statistically significant. The interaction with sex showed a statistical trend (p=0.07), with a rather stronger increase in risk related to SARS-COV2 infection in men (OR for SARSCOV2= 4.09 95%CI=3.22-5.20) than in women (OR SARS-COV2 =3.09 95%CI2.53-3.74).
DISCUSSION
In this retrospective study using the French database of 73.661 patients with hip fracture, a SARS-COV-2 infection within 30 previous days of surgery was associated with a 3-fold higher mortality rate (15.15%) compared to non-COVID-19 patients. This first large cohort is the first one that confirmed recent brief reports and meta-analysis that demonstrated an increased risks of 30-day mortality (32.23% COVID-19 + death vs. 8.85% COVID-19 - death) and inpatient mortality (29.33% vs. 2.62%) among COVID-19 + patients with odds ratio (OR) of 4.84 (95% CI: 3.13- 7.47, p<0.00001) and 15.12 (95% CI: 6.12-37.37, p<0.00001) [8,9].
With COVID-19 pandemic, performing surgery in the Covid setting has been widely debated. Indeed, all studies carried out during COVID-19 pleaded for postponing an elective surgery, when possible, for the patient, leading to recommend postponing surgical procedure in patients with recent SARS-COV-2 infection [6,7]. In patients with femoral neck fracture, this guideline could be challenged as postponing surgery induces an excess of mortality. As described recently, accelerated (<6h) vs standard care (<48h) in hip fracture surgery did not significantly lower the risk of mortality or a composite of major complications [2]. In the opposite, current guidelines pointed out that a delay of more than 48 hours was associated with an increased risk of mortality medical complications among patients with hip fracture [12-14]. In a national cohort of 73.661 elderly patients with hip fracture, the present study confirms a higher mortality rate in COVID-19 patients, considered as an additional mortality factor. In such conditions, the 15% mortality was 3-fold higher than in non-COVID-19 patients. Age and a poor baseline vital status were the other factors associated with a higher mortality rate.
Even if French national database is regularly checked meaning that it could be considered as to an exhaustive and accurate, using it is always challenging and can be a potential limitation of the study as SARS-COV2 patients were identified with diagnostic code. Indeed, asymptomatic, or infected patients earlier than 30 days before surgery might have been not tested and considered noninfected. However, this classification potential bias would have led to dilution effect and an underestimation of the effect of SARSCOV2 on mortality. On the other hand, given the purpose of the administrative database and its regular verification, we can assume that information on hip surgery is exhaustive and accurate during the study period.
The main finding of the present study is the absence of modulation of the effect of SARS-COV2 infection according to patient characteristics meaning that the SARS-COV-2 infection associated mortality risk remains constant whatever the patient and his(her) risk factors. Therefore, patients with multiple risk factors, the associated risk will be multiplied by 3 leading to a very high associated mortality rate. For instance, a patient with several risk factors and an already high absolute risk of death in the absence of SARS-COV2 infection (e.g., 20%) would have his absolute risk of death increased dramatically in the presence of infection (20%*3.4=68%). This may also be the population that would potentially benefit most from close monitoring for SARSCOV2 infection in the post-procedure period. Even the study focusses on 2020, our study period excluded the third wave (spring 2021) vaccination campaign effects and science updates, which might affect the primary outcome. Due to the deep impact of COVID-19 in health care organization, time before surgery such as hospital length of stay could have been impacted, compared to pre- COVID-19 outbreak.
In clinical practice, there are several reasons why a Covid patient’s hip fracture surgery might be postponed: the need for an additional respiratory assessment, waiting for the PCR test, unavailability of space in the hospital or operating theatre. Among adults undergoing hip fracture surgery and because Covid-19 infection was associated with a greater risk of 30-day mortality, a dedicated COVID-19 peri-operative pathway with early screening and surgical management would be an efficient key to enhanced postoperative recovery and mortality.
CONCLUSION
Recent or current SARS-COV2 infection is associated with a 3-fold higher mortality rate in elderly patients with hip fracture surgery. In this frail population, this excess mortality is an incentive not to defer intervention and to set up care pathways to enhance early rehabilitation.
REFERENCES
- Jiang M, Liu S, Deng H, Liang X, Bo Z (2021) The efficacy and safety of fast-track surgery (FTS) in patients after hip fracture surgery: A metaanalysis. J Orthop Surg Res 16(1): 162.
- HIP ATTACK Investigators (2020) Accelerated surgery versus standard care in hip fracture (HIP ATTACK): An international, randomized, controlled trial. Lancet 395(10225): 698-708.
- Veronese N, Maggi S (2018) Epidemiology, and social costs of hip fracture. Injury 49(8):1458-1460.
- Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, et al. (2017) Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA 318(20): 1994-2003.
- Berkwits M, Flanagin A, Bauchner H, Fontanarosa PB (2020) The COVID-19 pandemic and the JAMA Network. JAMA 324(12): 1159-1160.
- COVIDSurg Collaborative; GlobalSurg Collaborative (2021) Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia 76(6): 748-758.
- Zheng H, Hébert HL, Chatziperi A, Meng W, Smith BH, et al. (2020) Perioperative management of patients with suspected or confirmed COVID-19: Review and recommendations for perioperative management from a retrospective cohort study. Br J Anaesth 125(6): 895-911.
- Patralekh MK, Vain VJ, Iyengar KP, Upadhyaya GK, Vaishya R (2021) Mortality escalates in patients of proximal femoral fractures with COVID-19: A systematic review and meta-analysis of 35 studies on 4255 patients. J Clin Orthop Trauma 18: 80-93.
- Tripathy SK, Varghese P, Panigrahi S, Panda BB, Srinivasan A, et al. (2021) Perioperative mortality and morbidity of hip fractures among COVID-19 infected and non-infected patients: A systematic review and meta-analysis. Chin J Traumatol 1275(21): 00088-00092.
- Bellanger MM, Tardif L (2006) Accounting and reimbursement schemes for inpatient care in France. Health Care Manag Sc 9: 295-305.
- Toulouse E, Masseguin C, Lafont B, McGurk G, Harbonn A, et al. (2018) French legal approach to clinical research. Anaesth Crit Care Pain Med 37(6): 607-614.
- Simunovic N, Devereaux PJ, Sprague S, Gordon H, Guyatt G, et al. (2010) Effect of early surgery after hip fracture on mortality and complications: Systematic review and meta-analysis. CMAJ 182: 1609-1616.
- Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, et al. (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA 291(14): 1738-1743.
- Sheehan KJ, Sobolev B, Guy P (2017) Mortality by timing of hip fracture surgery: Factors and relationships at Play. J Bone Joint Surg Am 99(20): e106.
Article Type
Research Article
Publication history
Received Date: March 12, 2022
Published: April 18, 2022
Address for correspondence
Philippe Cuvillon, Division of Anaesthesia Intensive Care, Pain and Emergency Medicine, Nîmes University Hospital, France
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Yann G, Thierry B, Mamadou B, Amal B, Philippe C, et.al. Association Between Covid-19 Disease and Mortality After Hip Fracture Surgery in Elderly: A Multicentre National French Survey. 2022- 4(2) OAJBS.ID.000437.
Table 1: Characteristics of the subjects included in the study, overall and according to the presence of a hospitalization for COVID in the 30 days preceding admission for hip fracture surgery.
Table 2: Characteristics of the subjects according to death in the 30 days following admission for hip fracture surgery.
Table 3: Univariate and multivariate analyses of the association between subject characteristics and death at 30 days.