A Surprise Pulmonary Actinomycosis: A Case Report
ABSTRACT
Background: Pulmonary actinomycosis caused by actinomyces species; It is one of the rare infectious agents that can mimic
pathologies such as malignancy and tuberculosis in the lung. Due to nonspecific clinical and radiological findings, it is difficult to
diagnose in many cases.
Case presentation: A 81-year-old male patient with cough, sputum, fever and haemoptysis that started 3 days ago was admitted
to our outpatient clinic. He had no additional diseases other than hypertension and diabetes. Bronchoscopy was performed because
computed tomography of the thorax, which was taken due to accompanying recurrent haemoptysis, raised suspicion of malignancy.
Bronchoscopy findings were also suggestive of malignancy. In the pathology findings, actinomyces colonization was detected. In
the bronchial lavage and pathology findings, the growth of other agents and no findings in favor of malignancy were detected.
Pulmonary actinomycosis was accepted and high-dose penicillin was started, and the patient’s complaints regressed in a short time.
In the 2nd month, the radiological findings completely improved.
Conclusion: Pulmonary actinomycosis should be kept in mind in the differential diagnosis of treatment refractory pneumonia
in cases where malignancy is suspected.
KEYWORDS
Actinomycosis; Haemoptysis; Malignancy
ABBREVIATION
CT: Computed Tomography; EZN: Ehrlich Ziehl Nelsen
BACKGROUND
Actinomyces is a non-contagious, facultative anaerobic, grampositive bacterium with a filamentous shape, characterized by slow growth [1]. It is usually found in the oral cavity, dental caries, and tonsils. Actinomycosis is a rare infectious bacterial disease caused by actinomyces species. Bacteria of actinomyces species belong to the normal human flora and have been detected in the oral cavity, gastrointestinal tract and female genital tract. The development of actinomycosis results from disruption of the mucosal barrier, which allows the spread of bacteria, causes endogenous infection and affects multiple organs [2]. The most common forms of actinomycosis are cervicofacial and abdominopelvic actinomycosis. The pulmonary form is the third most common type of actinomycosis, estimated to be accounting for approximately 15% of the total burden of the disease.
The pulmonary form of actinomycosis may result from aspiration of oropharyngeal or gastrointestinal secretions [3]. The clinical presentation of pulmonary actinomycosis is varied, including cough, fever, haemoptysis, and weight loss. In addition, the low specificity of imaging findings of pulmonary actinomycosis complicates the diagnosis. As in the case we shared, it is difficult to distinguish this infection from other diseases such as lung cancer, tuberculosis and aspergillosis [4].
CASE PRESENTATION
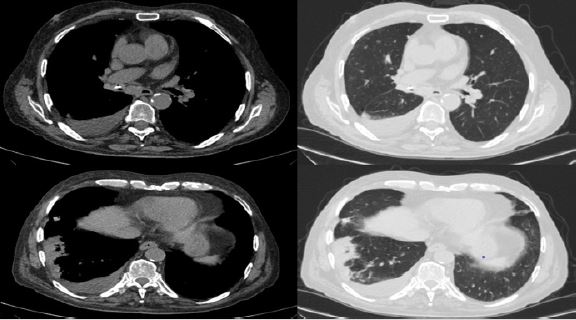
81 years old male patient; He applied to the outpatient clinic with complaints of cough, sputum, occasional fever and recurrent haemoptysis for 3 days. He had no additional complaints. Pulse oximetry saturation was measured as 92% in room air. Vital signs were stable. Breath sounds were decreased in the lower right zone on auscultation. Oral hygiene was observed as normal. No abnormality was detected in other examination findings. He had known hypertension and diabetes diseases. He had no history of smoking. No feature was found in his family history. In laboratory techniques, white blood cell: 10.94x10^3/μL, hemoglobin: 12.1 g/dL, platelet: 210x10^3/μL, C-reactive protein: 15 mg/dL were measured. Thorax CT was requested because of haemoptysis. On thorax CT, pleural effusion and accompanying compression atelectasis in the right lung, a partially calcified lesion obstructing the right lung intermediate bronchus entrance and areas of pneumonic consolidation in the lower lobe were observed (Figure 1).
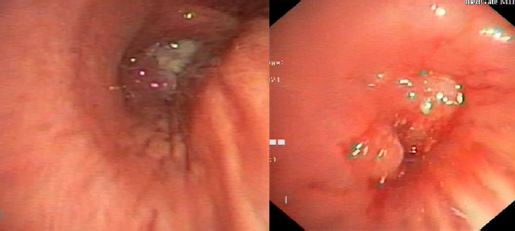
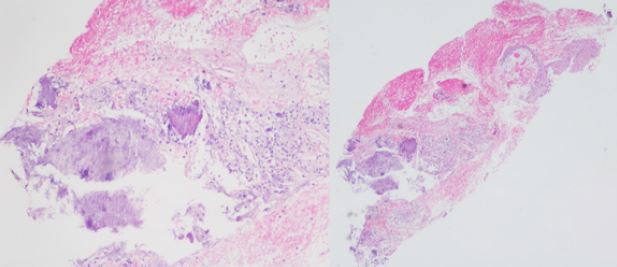
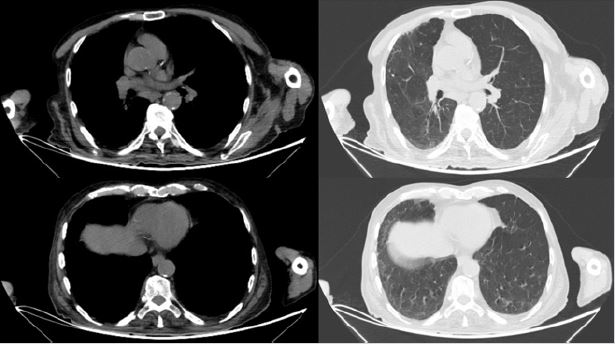
Bronchoscopy was planned because the patient’s radiological findings aroused suspicion of post obstructive pneumonia and malignancy. Intermediary bronchial access in bronchoscopy; It was observed to be occluded with a polypoid lesion with purulent secretion (Figure 2). Other lobe entrances and segments were observed open. Bronchial biopsies from the lesion and bronchial lavages from the intermediate bronchus were taken. Tuberculosis culture and EZN staining were negative in the samples taken. There was no growth in bacterial and fungal cultures of bronchial lavage. In the pathology report, it was stated that actinomyces colonization was observed and no findings in favor of malignancy were found (Figure 3). The patient, who was accepted as pulmonary actinoicosis, was started on high dose penicillin treatment and followed up. His complaints regressed in the early period. In the control thorax CT taken 8 weeks later, it was observed that the parenchymal findings regressed, and the right intermediate bronchial system was completely opened (Figure 4).
DISCUSSION
Pulmonary actinomycosis is a rare infection caused by actinomyces. It is a suppurative, granulomatous disease usually caused by inhaled oropharyngeal secretions. Long term smokers often have poor oral hygiene, which may be a factor in the development of actinomyces infection [1]. In addition, chronic lung diseases such as bronchiectasis and chronic obstructive pulmonary disease, hematological diseases such as alcoholism, diabetes, leukemia, human immunodeficiency virus infection, use of immunosuppressive agents such as corticosteroids and anti-TNF agents have been associated with the development of pulmonary actinomycosis [5]. There was no smoking in our patient. There was no additional disease except diabetes and hypertension.
Pulmonary actinomycosis remains an important problem for clinicians because of the no specificity of symptoms and the similarity of the disease to other chronic suppurative pulmonary diseases and malignancies. Fever, cough, sputum, shortness of breath, weakness, weight loss, night sweats, chest pain and haemoptysis are the main symptoms [6,7]. Our case had similar complaints. When the disease is evaluated in terms of laboratory findings; Normochromic anaemia, leucocytosis and mild C-reactive protein increase can be observed [3-8]. Various features have been described on thorax CT in pulmonary actinomycosis, particularly air bronchogram consolidation, lobar consolidation, ground glass opacification, and pleural effusions. Pleural thickening, hilar lymphadenopathy and necrotic mass may be seen [9]. Bronchoscopy findings of endobronchial actinomycosis are also non-specific. In the past reports, endobronchial actinomycosis may be bronchoscopically with granular thickening and partial obstruction of the bronchi, submucosal or exophytic mass appearances with or without necrotic material; It has been reported to mimic lung cancer and tuberculosis [2,10,11].
In our case, both radiological and bronchoscopy findings were suggestive of malignancy. Microbiological diagnosis requires immediate sample handling and prolonged bacterial culture (5-20 days) under anaerobic conditions. In most cases of actinomycosis, bacterial confirmation is not obtained as a result of insufficient incubation time, or previous antibiotic therapy [12]. The optimum approach in diagnosis is pathological examination of the samples taken by biopsy and the production of microorganisms in culture [13]. The main treatment is high dose intravenous penicillin (usually for 2-6 weeks) 18-24×10⁶ units of penicillin per day) followed by oral penicillin V (or amoxicillin) for an additional 6-12 months [3- 14]. Metronidazole, aminoglycosides, co-trimoxazole, aztreonam and fluoroquinolones have weak or no activity against actinomyces species [15]. The prognosis of the disease is generally good. However untreated pulmonary actinomycosis; It can cause serious complications such as empyema, costal erosion, and mediastinal invasion that can progress to the heart and cause pericarditis [16].
CONCLUSION
Pulmonary actinomycosis is difficult to distinguish from tuberculosis and neoplasia both clinically and radiologically. It is a rare infectious disease without specific symptoms. Therefore, the presence of pulmonary actinomycosis should be considered in the differential diagnosis of patients with suspected tuberculosis or neoplasia. Awareness should be increased in endobronchial lesion management and in cases with suspected endobronchial actinomycosis. As in our case, endobronchial lesions may regress with penicillin treatment. In the diagnosis, histopathological examination or production of bacteria in culture is necessary under appropriate conditions.
AUTHORS’ CONTRIBUTION
GK writes first version of the manuscript, and MD completed all documents. GK, EA and MD were responsible for the treatment of the patient. MD, EA, EC supervised the treatment and the completion of this case report. EC commented on pathology. All authors read and approved the final manuscript.
REFERENCES
- Ding X, Sun G, Fei G, Zhou X, Zhou L, et al. (2018) Pulmonary actinomycosis diagnosed by transbronchoscopic lung biopsy: A case report and literature review. Exp Ther Med 16(3): 2554-2558.
- Oikonomidis P, Fousekis F, Kotsaftis P, Pilios I, Dimas D, et al. (2019) A case of pulmonary actinomycosis presented with endobronchial involvement. Respir Med Case Rep 28:100930.
- Mabeza GF, Macfarlane J (2003) Pulmonary actinomycosis. Eur Respir J 21(3): 545-551.
- Kim SR, Jung LY, Oh IJ, Kim YC, Shin KC, et al. (2013) Pulmonary actinomycosis during the first decade of 21st century: cases of 94 patients. BMC Infect Dis. 13: 216.
- Valour F, Senechal A, Dupieux C, Karsenty J, Lustig S, et al. (2014) Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist 7: 183-197.
- Frank P, Strickland B (1974) Pulmonary actinomycosis. Br J Radiol 47: 373-378.
- Barikbin P, Grosser K, Hahn G, Fischer R, Suttorp M (2007) Thoracic actinomycosis imitating a malignant chest wall tumor diagnosis: pulmonary actinomycosis. J Pediatr Hematol Oncol 29: 345-346.
- Ozgun S, Yaprak Bayrak B, Ciftci Kusbeci T, Ilgazlı A (2021) A rare case of pulmonary infection: Endobronchial actinomycosis. Respir Case Rep 10(1): 23-26.
- (2006) Toracic actinomycosis: CT features with histopathologic correlation. AJR Am J Roentgenol 186(1): 225-231.
- Farrokh D, Rezaitalab F, Bakhshoudeh B (2014) Pulmonary actinomycosis with endobronchial involvement: a case report and literature review. Tanaffos 13(1): 52-56.
- Jin SL, Lee HP, Kim JI, Chin JY, Choi SJ, et al. (2000) A case of endobronchial actinomycosis. Korean J Intern Med 15(3): 240-244.
- Bennhoff DF (1984) Actinomycosis: diagnostic and therapeutic considerations and a review of 32 cases. The Laryngoscope 94(9): 1198-1217.
- Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, et al. (2022) Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist 7(2014): 183-197.
- Sobajima T, Asano F, Tsuzuku A, Murakami A, Masuda A, et al. (2015) A case of pulmonary actinomycosis associated with aspiration of cedar leaves. J Bronchology Interv Pulmonol 22: 259-262.
- Boyanova L, Kolarov R, Mateva L, Markovska R, Mitov I (2015) Actinomycosis: a frequently forgotten disease. Future Microbiol 10(4): 613-628.
- Wong VK, Turmezei TD, Weston VC (2011) Aktinomikoz. BMJ 343: d6 099.
Article Type
Case Report
Publication history
Received Date: August 31, 2022
Published: December 14, 2022
Address for correspondence
Gökhan Karakurt MD, Department of Chest Diseases, Faculty of Medicine, Medipol University Hospital, Turkey
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Gökhan K, Mustafa D, Engin A, Elif C. A Surprise Pulmonary Actinomycosis: A Case Report. 2022- 4(6) OAJBS.ID.000529.
Figure 1: Initial radiological findings. On thorax CT a partially calcified lesion and pleural effusion obstructing the intermediary bronchus entrance in the right lung and consolidation areas, pleural effusion and accompanying compression atelectasis in the lower lobe of the right lung.
Figure 2: Bronchoscopy findings. In bronchoscopy, polypoid lesion covered with bronchial wall thickening and purulent secretion in the continuation of the intermediate bronchus entrance.
Figure 3: Pathological findings at x10 and x4 magnification. Inflammatory cell infiltration and actinomyces colonization.
Figure 4: Radiological findings after treatment. Endobronchial lesion, parenchymal consolidations and pleural effusion regressed radiologically in the 8 weeks after treatment.