The Blistered Rachis-Spinal Synovial Cyst
PREFACE
Facet joint cyst emerges as a circumscribed lesion surrounding facet joint abutting vertebral foramina or within epidural or
paravertebral region. Spinal synovial cyst is an infrequently discerned, benign, degenerative, space-occupying lesion of the vertebral
column adjoining facet joints. An extra-dural, soft tissue mass permeated with liquid content appears confined to medial border
of deteriorated facet joint. Aforesaid lesion is denominated as spinal synovial cyst and may be additionally designated as a “juxtafacet
cyst”. Spinal cystic lesions originate from diverse ligamentous and synovial structures. Spinal synovial cyst can emerge from
facet joint, protrudes beyond joint margin and is pervaded with serous, mucoid or haemorrhagic fluid. Spinal synovial cyst can be
bilateral and engender cogent radicular symptoms.
Spinal synovial cyst is usually confined to lumbar vertebral region and characterizes synovial cysts and ganglion cysts configured
within extradural region of spinal column. Intra-spinal synovial cysts are uncommon. However, persisting lower back pain and
reoccurring radicular pain may arise due to degenerative alterations of the vertebral column, thereby necessitating a surgical fusion
procedure. Clinical symptoms of mild to moderate intensity are appropriately treated and meliorated with minimally invasive
therapies such as cyst aspiration and fluoroscopy guided infiltration with corticosteroids. Cyst resection, decompression of neural
structures and accompanying vertebral fusion is recommended for concomitant segment instability.
ABBREVIATIONS
CT: Computerized Tomography; MRI: Magnetic Resonance Imaging; PEEK: Polyether Ether Ketone; TLIF: Transforaminal Lumbar Interbody Fusion; STIR: Short Tau Inversion Recovery
DISEASE CHARACTERISTICS
The mobile lumbar spine is prone to instability, thus spinal synovial cyst is predominant within lumbar spinal region. In contrast to anterior region, posterior lumbar lesions are frequent. Nevertheless, few spinal synovial cysts emerge within cervical and thoracic spine. An estimated ~ half the synovial facet cysts appear as an incidental lesion and around half [50%] of spinal synovial cysts are symptomatic. Facet cysts are common in individuals delineating severe facet degeneration and joint instability [1,2].
Spinal synovial cyst is categorized into:
a. Synovial cyst which exhibits a distinctive synovial layer
b. Pseudocyst which is derived from degeneration of
ligamentum flavum
c. Pseudocyst, which is devoid of a synovial layer, as encountered
with ganglion cyst [1,2].
Spinal synovial cyst is posited to arise from segmental instability and degenerative alterations and hypertrophy of facet joint. Of debatable genesis, spinal synovial cyst is postulated to arise as a complex, preliminary degeneration of intervertebral disc. Elevated pressure and facet hypertrophy appears associated with degenerative spondylolisthesis, features which contribute to instability within facet joint and pertinent clinical symptoms [1,2].
Clinical Elucidation
Clinical manifestations are associated with repercussions and range from an asymptomatic lesion to occurrence of lumbar pain, radicular pain, an infrequent radicular neurological deficit or cauda equina syndrome. Generally asymptomatic, spinal synovial cyst engenders symptoms of variable severity. Radicular pain is frequently observed along with lumbar pain, sensory deficit, neurogenic claudication and limb paresis. The pain may gradually worsen [1,2].
Spinal synovial cyst can induce low back pain, lumbar radiculopathy and neurological deficits. Radiating spinal or radicular pain and hypoesthesia in the absence of motor deficit may ensue. Lateral movements of lumbar spine may be painful and rotational movement may be restricted. Spinal synovial cyst simulates clinical symptoms of disc herniation and spinal stenosis. Facet cyst may compress the thecal sac and abutting nerve roots. Synovial cyst emerging within the capsule of lumbar zygapophysial joint can generate clinical symptoms simulating an extradural space-occupying lesion [3,4].
Lumbar pain and radicular pain un-associated with motor impairment may be intense within specified segments. Bilateral facet joint cysts are infrequent and engender cogent radicular symptoms as lumbar pain and radicular pain. Also, spinal synovial cysts confined to upper lumbar synovial facet joints are uncommon. Spinal synovial cyst may be infrequently associated with spontaneous, acute intra-cyst haemorrhage which can engender significant nerve root compression. Also, haemorrhagic synovial cyst may arise on account of administration of anticoagulants [3,4].
Spontaneous or degenerative joint disorders or an obscure aetiology may concur to engender haemorrhagic metamorphosis of spinal synovial cyst. Segmental instability with glide and degenerative alterations within the spinal column may generate spinal synovial cyst which may be associated with hypertrophy, vacuum phenomenon, asymmetric changes and facet tropism [3,4].
Histological Elucidation
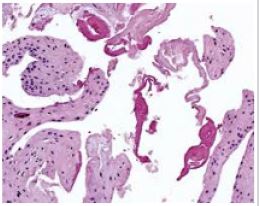
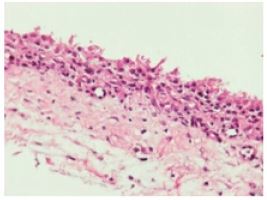
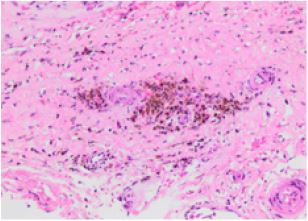
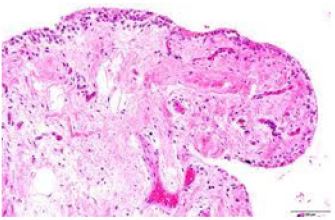
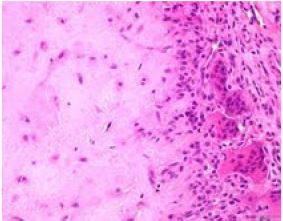
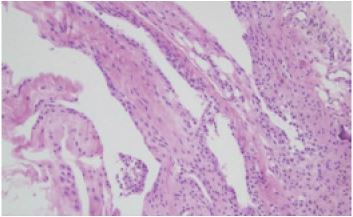
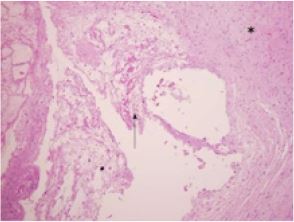
Upon gross examination, spinal synovial cyst is layered with fibrous tissue and permeated with clear, mucoid or xanthochromic fluid. A dark-brown, haemorrhagic, soft tissue mass of variable magnitude appears admixed with fragments of bone. Upon microscopy, segments of fibrous tissue are intermingled with bony trabeculae. Papillae-like configurations appear indicative of synovium. Hemosiderin pigment deposits are suggestive of remote or distant haemorrhage. Spinal synovial cyst may be layered with fibrous tissue along with or an absence of a synovial lining. An inflammatory cell exudate, granulomatous inflammation or malignant metamorphosis is usually absent. Spinal synovial cyst is layered with an epithelium akin to synovial epithelium which appears contiguous with the joint capsule [5,6]; (Figures 1-7).
Differential Diagnosis
Subjects depicting progressive dorso-lumbar pain and radicular symptoms necessitate assessment for symptomatic lumbar facet cysts. Spinal synovial cyst requires a segregation from spinal degenerative processes and space-occupying lesions of the spinal canal such as herniation of lumbar disc, hypertrophy of ligamentum flavum or facet joint hypertrophy associated with stenosis or joint instability [5,6].
Investigative Assay
Upon standing and dynamic plain radiography, lumbar instability and laminar inclination can be observed. Computerized tomography (CT) is adopted for assessing possible segmental instability and angle of laminar inclination along with degenerative alterations and facet tropism. Computerized tomography can discern degenerative facet modifications and vacuum phenomenon of the lumbar region with facet tropism. Magnetic resonance imaging [MRI] is an optimal investigative modality for evaluating characteristics, localization, magnitude, liquid constituents of spinal synovial cyst, concurrence with neural elements and degenerative alterations of the intervertebral disc. Upon magnetic resonance imaging (MRI), spinal synovial cyst appears as a well circumscribed, epidural lesion. Magnetic resonance imaging exhibits moderate to severe degenerative intervertebral disc alterations of lumbar vertebrae. MRI exemplifies generalized degenerative spondyloarthropathy of the lumbar spine along with spinal synovial cyst which restricts the vertebral canal and compresses dural sac and lateral recesses of adjacent nerve roots [7,8].
Upon T1 weighted imaging the cyst exhibits decimated signal intensity and upon T2 weighted imaging the lesion appears hyperintense with enhanced signal intensity. Upon short tau inversion recovery (STIR) sequences, synovial cyst of lumbar facet joint appears hyper-intense. In contrast, spinal synovial cyst associated with intra-cyst haemorrhage appear hyper-intense upon T1 weighted imaging and hypo-intense upon T2 weighted imaging [7,8].
Spinal synovial cyst can be classified with standing lateral radiographs and MRI pertaining to proportionate compression of spinal canal and grade of spondylolisthesis. Aforesaid classification is efficacious in segregating individuals with possible cyst reoccurrence following decompressive surgery, especially in subjects depicting spondylolisthesis with a degree of slippage ≥ 15% [9,10].
Therapeutic Options
Spinal synovial cyst can be reduced or may undergo spontaneous resolution with appropriate rest and immobilization. Optimal therapy of spinal synovial cyst remains debatable although cogent strategies employed are conservative management, intervention techniques as image-guided epidural corticosteroid injections, direct aspiration of the cyst for persistent radiculopathy or surgical manoeuvers as an open or endoscopic cystectomy, spinal canal decompression and spinal bone fusion, especially in instances of wide facet joint resection or instability. Lumbar laminectomy and surgical excision of cyst can be suitably adopted [9,10].
Variable treatment strategies are contingent to cogent clinical symptoms, localization and characteristics of the lesion, associated segmental instability, degenerative alterations within the spinal cord and individual preferences. Non-surgical treatment strategies are comprised of percutaneous techniques such as cyst aspiration, corticosteroid infiltration within the cyst or cyst rupture. Percutaneous aspiration of non-haemorrhagic spinal synovial cyst and infiltration of corticosteroids or local anaesthetic agents can ameliorate radicular pain for a brief duration [11,12].
Preliminary, conservative management with physiotherapy and non-steroidal, anti-inflammatory drugs [NSAIDs] or analgesics may be accompanied by inadequate therapeutic outcomes. Subsequently, percutaneous cyst aspiration and steroid infiltration of facet joint under fluoroscopic guidance can be adopted, manoeuvres which meliorate radicular symptoms. Incriminated subjects may be unresponsive to medical management. Nevertheless, degenerative alterations of intervertebral discs and facet joints necessitate fusion surgery. The current, standard treatment strategy for lumbar or haemorrhagic, spinal synovial cyst is surgical extermination with decompression of circumscribing neural structures [11,12].
Lumbar synovial cyst associated with intra-cystic haemorrhage is optimally treated with surgical eradication of the cyst with decompression. Acute clinical symptoms necessitate prompt surgical intervention. Nevertheless, neurological disability may remain. Persistence of lumbar pain and reappearance of radicular pain manifest as indications for surgical intervention. Procedures such as hybrid fusion of lumbosacral vertebrae through unilateral transforaminal lumbar interbody fusion (TLIF) approach can be adopted. Also, implicated facet joints can be strengthened with interbody polyether-ether-ketone (PEEK) implants, pedicle screws or autologous bone [13,14]. Standing and dynamic radiographs are optimal in evaluating laminar inclination angle and segmental instability of the vertebral column. Open or endoscopic cyst excision devoid of joint fusion may be optimal in individuals demonstrating an absence of segmental instability. However, proportionate facetectomy can be adopted in order to circumvent cyst reoccurrence. Besides, therapeutic indications may be contingent to cyst location, as discerned with MRI. Type 1 or medial facet joint cysts with compression of dura and non-compressed nerve roots can be optimally managed with ipsilateral laminectomy. Spinal synovial cysts compressing the dura and nerve roots can be categorized as type 2 or mediolateral cyst [13,14].
Intra-canal spinal synovial cyst engendering radicular compression are categorized as type 3 or lateral cysts and can be subjected to contralateral facetectomy with preservation of facet joints. Decompression of neural elements with instrumented joint fusion can be adopted for treating concomitant spondylolisthesis or facet arthrosis and is associated with proportionately decimated cyst reoccurrence. Complications such as rent within the dura, pseudoarthrosis and secondary infection along with perioperative morbidity may be enhanced with diverse surgical manoeuvres. Fixation is recommended and is employed contingent to joint instability and accompanying cyst reoccurrence. Besides, it is required to decimate pain and enhance functional activity [13,14].
REFERENCES
- Liawrungrueang W, Choksuphan D, Torphong B (2022) Can acute radiculopathy be caused by upper lumbar haemorrhagic synovial cyst spinal compression in the elderly? International Journal of Surgery Case Reports 93: 107002.
- David RP, José RV, Ana VG (2020) An unusual case of radicular pain caused by bilateral lumbar synovial cyst: A case report and review of the literature. Case Reports in Orthopaedics 8821332.
- Janssen SJ, Ogink PT, Schwab JH (2018) The prevalence of incidental and symptomatic lumbar synovial facet cysts. Clinical Spine Surgery 31(5): E296-E301.
- Chebib I, Chang CY, Joseph HS, Darcy AK, Vikram D, et al. (2018) Histopathology of synovial cysts of the spine. Histopathology 72(6): 923-929.
- Hohenberger C, Brawanski A, Winfried OU, Julius H, Florian Z, et al. (2019) Degenerative symptomatic spinal synovial cysts: clinical presentation and functional outcome. Journal of Clinical Neuroscience 62: 112-116.
- Nordmann NJ, Michael AP, Jose AE (2019) Resolution of symptomatic lumbar synovial cyst after traumatic event. World Neurosurgery 128: 69-71.
- Wun K, Hashmi SZ, Joseph M, Andrew DS, Karina MK, et al. (2019) The variability of lumbar facet joint synovial cyst recurrence requiring revision surgery after decompression-only and decompression/fusion. Clinical Spine Surgery 32(10): E457-E461.
- Rosenstock T, Vajkoczy P (2020) New classification of facet joint synovial cysts. Acta Neurochirurgica 162(4): 929-936.
- Themistoklis KM, Papasilekas TI, Konstantinos AB, Dimitrios AG, Eustathios NV, et al. (2018) Spinal synovial cysts. A case series and current treatment options. Journal of Clinical Neuroscience 57: 173-177.
- Splavski B, Ante R, Ivan B, Ivan K, Domagoj G, et al. (2019) Lumbar spine synovial cyst: a case series report and review of surgical strategies. Acta Clinica Croatica 58: 491-496.
- Boody BS, Savage JW (2016) Evaluation and treatment of lumbar facet cysts. Journal of the American Academy of Orthopaedic Surgeons 24(12): 829-842.
- Bruder M, Cattani A, Florian G, Christian D, Matthias S, et al. (2017) Synovial cysts of the spine: long-term follow-up after surgical treatment of 141 cases in a single-centre series and comprehensive literature review of 2900 degenerative spinal cysts. Journal of Neurosurgery Spine 27(3): 256-267.
- Kim KH, Kim SY, Hwoe GO, Tae KK (2019) A staged treatment of symptomatic lumbar intraspinal synovial cysts. Pain Physician 22(5): E451-456.
- Mobbs R, Campbell R, Kevin P (2018) Neuro Spine Surgery Research Group (NSURG) classification system for grading lumbar synovial cysts. Orthopaedic Surgery 10(1): 3-7.
Article Type
Case Report
Publication history
Received Date: June 02, 2022
Published: June 14, 2022
Address for correspondence
Anubha Bajaj, Consultant Histopathology, AB Diagnostics, India
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Anubha B. The Blistered Rachis-Spinal Synovial Cyst. 2022- 4(3) OAJBS. ID.000458.
Figure 1: Spinal synovial cyst demonstrating papillary structures layered with synovium-like epithelium with subjacent fibrous connective tissue and focal haemorrhage.
Figure 2: Spinal synovial cyst depicting an attenuated wall layered with multitudinous, focally ciliated epithelium with microvilli superimposed upon fibrous connective tissue.
Figure 3: Spinal synovial cyst exhibiting circumscribing fibrous connective tissue with foci of hemosiderin pigment deposition.
Figure 4: Spinal synovial cyst delineating papillary structures coated with synovial epithelium and subjacent connective tissue with focal haemorrhage.
Figure 5: Spinal synovial cyst demonstrating cavity layered with ciliated columnar epithelium superimposed upon fibrous connective tissue.
Figure 6: Spinal synovial cyst exemplifying a cyst wall coated with cuboidal epithelium with underlying fibrous connective tissue.
Figure 7: Spinal synovial cyst enunciating papillary configuration lined with columnar epithelium along with circumscribing fibrous connective tissue.