Role of Magnetic Resonance Imaging in the Diagnosis and Prognosis of Cardiomyopathy
ABSTRACT
Background: Magnetic resonance is a physical property of a nucleus that has an odd number of protons or neutrons. The most
abundant such nucleus in the body is the hydrogen proton. Magnetic Resonance is a technique that takes images of the heart in
motion throughout the cardiac cycle and displays the heart’s motion in a cine loop.
Methodology: A systematic review was carried out through various databases from January 2013 to September 2022;
The search and selection of articles was carried out in indexed journals in English. Key words were used: Magnetic Resonance,
Cardiomyopathies, Indications, Prognosis.
Results: One of the main research tools that present greater clinical application in a safe and complete way is magnetic resonance
imaging. It has important applications in acute myocardial infarction, dilated cardiomyopathy, hypertrophic and arrhythmogenic
right ventricular cardiomyopathy, among other heart diseases.
Conclusions: This review offers up-to-date and detailed information on the main indications and contraindications of
Cardiovascular Magnetic Resonance as well as its important applications in heart failure, one of the most frequent cardiovascular
pathologies and among other cardiomyopathies.
KEYWORDS
Magnetic resonance; Cardiomyopathies; Indications; Prognosis
INTRODUCTION
Magnetic resonance is a physical property of a nucleus that has an odd number of protons or neutrons. The most abundant such nucleus in the body is the hydrogen proton. Cardiovascular MRI can delineate cardiovascular structures with adequate spatial resolution and tissue contrast [1]. Some sequences are specially designed to image cardiovascular structures. To enhance the signal from the myocardial or vascular wall, it is necessary to suppress the signal from blood and fat. To do this, inverting radio frequency priming pulses are added to suppress the blood signal, resulting in an image that looks like “dark blood.” Another saturation or inversion of radio frequency pulses can be added to suppress the signal from the fat, resulting in an image with a “dark blood and dark fat” appearance. The dark blood technique uses double-inverted recovery priming pulses to nullify the blood signal and outlines cardiac and vascular structures with the darkened blood [2]. This dark blood image has many clinical applications, which help to identify vascular anomalies, such as congenital anomalies, aortic or vascular disease, cardiovascular tumours, myocarditis, among other cardiomyopathies [3]. The heart has a strong task of pumping blood through two circulations, a greater circulation, which is the systemic circulation to be able to supply oxygen, nutrients, and other components to the peripheral tissues, and the smaller circulation, which is the pulmonary circulation, to be able to supply itself with oxygen and expel CO2. Magnetic Resonance is a technique that takes images of the heart in motion throughout the cardiac cycle and displays the heart’s motion in a cine loop [4,5]. Magnetic Resonance can evaluate the global function of the left and right ventricle. Ventricular volume can be estimated by summing several parallel sub-volumes in the short-axis view. This approach has been shown to be highly accurate and reproducible, but requires software and human intervention to define the endocardial contour on each cine image [6]. Magnetic Resonance has become a standard clinical technique to visualize myocardial scarring. It allows us to identify the spatial location and extension of the scar, whose information can facilitate the differential diagnosis of cardiomyopathy. Ischemic cardiomyopathy and nonischaemic cardiomyopathy have different etiologist and specific patterns of hyperenhancement. Therefore, we can distinguish ischemic cardiomyopathy from non-ischemic cardiomyopathy based on different enhancement patterns. In addition, specific enhancement patterns have been characterized in different etiologist of nonischaemic cardiomyopathy such as hypertrophic cardiomyopathy, arrhythmogenic right ventricular dysplasia, Anderson-Fabry disease, amyloidosis, sarcoidosis, and acute myocarditis [7]. Another of the functions of Cardiovascular Magnetic Resonance is myocardial perfusion imaging, this is an imaging technique designed to assess myocardial microcirculation [8]. Myocardial perfusion is generally performed in states of rest and stress. Unlike the resting state, the stress state is pharmacologically induced by a vasodilator such as adenosine or dipyridamole, which causes myocardial hyperaemia and increases perfusion [9]. Another of the applications of Magnetic Resonance is angiography. The ultimate goal of coronary MRI angiography is to diagnose luminal stenosis. The goal is challenging because the diameter of a coronary artery does not exceed 5 mm and the arteries always move with the movement of the heart and breathing [10]. To date it is still important and challenging to safely and reliably perform Cardiovascular Magnetic Resonance imaging. With the rapid progress of MRI technologies, many new methods have been developed to diagnose cardiovascular diseases. Therefore, it is convenient to carry out this work. In order to provide updated and detailed information on the main indications and contraindications of Cardiovascular Magnetic Resonance as well as its important applications in cardiovascular insipience, one of the most frequent cardiovascular pathologies.
MATERIALS AND METHODS
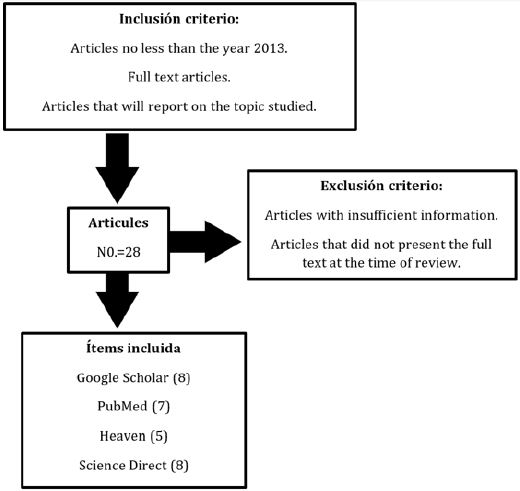
In this study, a systematic review was carried out, within the databases that were implemented, we found the following PubMed, Scioli and ScienceDirect, among others. Only journals that were in the English language between the years 2012 and 2022 were accepted. As keywords, according to the DeCS and MeSH methodology, we included the following terms: Magnetic Resonance; Cardiomyopathies; Indications; Forecast. In this review, 92 original and review publications related to the subject studied were identified, of which 28 articles met the inclusion criteria, articles that were in a range of not less than the year 2013, that were full-text articles and that report on the topic studied. Within the exclusion criteria we find the articles that did not have sufficient information and that did not present the full text at the time of review. In Figure. 1, we can identify a diagram of the implemented methodology.
RESULTS
Magnetic Resonance and Heart Disease
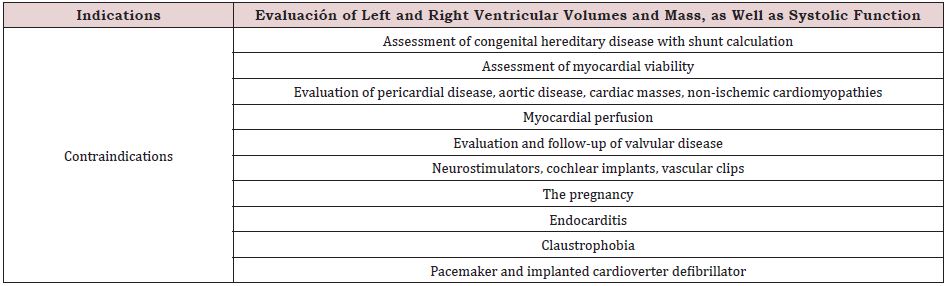
One of the main research tools that present greater clinical application in a safe and complete way is magnetic resonance imaging. It is one of the most accurate tools to quantify ventricular volume, function, and mass in both congenital and acquired heart disease [11]. Cardiovascular MRI has evolved over the past decade to become a valuable tool for the diagnosis and treatment of a broad spectrum of cardiovascular disorders. In Table 1 we can identify the main implications [12,13].
Ventricular Volumes, Ejection Fraction and Myocardial Mass
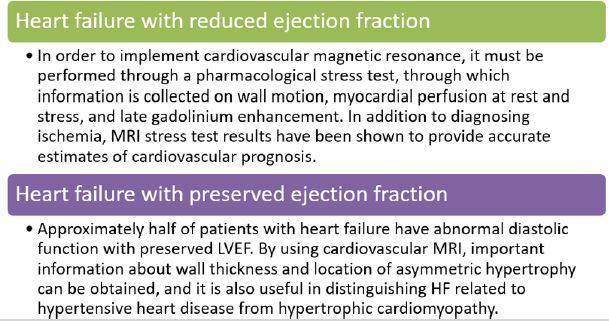
One of the studies that quantifies these parameters with greater precision is magnetic resonance imaging. ECG-triggered “bright blood” cine sequences are used, while holding breath, to obtain a “stack” of contiguous slices of the left ventricular short axis 5 to 10 mm thick [14]. Cardiovascular MRI is a tomographic technique that uses volumetric quantification based on Simpson’s rule: the volume of a complex structure (ventricle) is equal to the sum of less complex sub-volumes (short axis slices) [15]. Endocardial and epicardial contours are drawn during post-processing (“offline”, after MRI examination), generating end-diastolic, end-systolic and systolic volumes, ejection fraction (stroke volume divided by end-diastolic volume), and myocardial mass (myocardial volume multiplied by the specific weight of the muscle) [16]. Cardiovascular MRI yields more accurate values for left ventricular parameters than planar imaging methods and is the most reliable way to assess regional and global right ventricular function. In Figure 2. We can demonstrate the application of magnetic resonance in heart failure with reduced and preserved ejection fraction [17,18].
Application in Acute Myocardial Infarction
During myocardial infarction, a “wave” of cell death moves from the endocardium to the epicardium, resulting in the replacement of a variable amount of myocardium with scarring. Impaired myocardial contraction in ischemic cardiomyopathy is not always a consequence of myocardial fibrosis alone [19]. In some cases, there is myocardial “stunning”: reduced contraction initially after myocardial infarction despite successful reperfusion of the culprit artery, followed by spontaneous recovery within weeks [20]. In other cases, there is myocardial “hibernation”: impaired contraction in the absence of significant scarring, a consequence of flow-limiting coronary stenosis with chronic ischemia [21,22]. In patients with ischemic cardiomyopathy, the left ventricular ejection fraction is a more powerful prognostic factor than the number of diseased coronary arteries. Accurate discrimination between viable and nonviable myocardium is important in deciding on treatment strategy in ischemic cardiomyopathy. With delayed contrast enhancement (DCE), a cardiovascular MRI technique that uses Gd-PCM, we can directly visualize areas of acute or chronic myocardial infarction or enema. The mechanism is presumed to be a combination of washout/delayed washout kinetics and different volumes of distribution of Gd-PCM in regions of myocardial enema, necrosis, or fibrosis compared to normal areas [23]. Dysfunctional myocardial regions with less than 50% transmural infarct extension have a good chance of functional recovery after myocardial infarction or coronary artery bypass surgery [24].
Application in Dilated Cardiomyopathy
Clinically, it is important to differentiate between two events, between dilated and ischemic cardiomyopathy, especially in patients presenting with new-onset heart failure. Coronary angiography is often performed to provide a diagnosis, because patients with ischemic cardiomyopathy have a shorter survival time than patients with dilated cardiomyopathy and may benefit from coronary revascularization therapy. Myocardial scarring with an “ischemic” pattern of DCE distribution is present in the majority of patients with ischemic cardiomyopathy, but in less than 15% of patients with dilated cardiomyopathy, which is consistent with findings from autopsy studies demonstrating a visible scar in 14% of cases [25].
Application in Hypertrophic and Arrhythmogenic Cardiomyopathy of the Right Ventricle
Cardiovascular MRI can diagnose hypertrophic cardiomyopathy by demonstrating the distribution of hypertrophy and functional consequences (dynamic outflow obstruction and mitral valve regurgitation) [26]. Cardiovascular MRI can more accurately demonstrate the site and extent of hypertrophy, especially in the apical region. Arrhythmogenic right ventricular cardiomyopathy is characterized by progressive fibrofatty replacement involving variable regions of the right and left ventricle. Cardiovascular MRI is useful in diagnosing the condition when right ventricular abnormalities, such as decreased global or regional wall motion or aneurysms, correspond to areas of fibrofatty infiltration detected on T1-weighted imaging.
DISCUSSION
The cardiovascular system is made up of the heart and its blood vessels. A wide range of problems can arise within the cardiovascular system, some of which include endocarditis, rheumatic heart disease, and conduction system abnormalities. Cardiovascular disease, also known as heart disease, refers to the following 4 entities: coronary artery disease which is also known as coronary heart disease, cerebrovascular disease, peripheral arterial disease, and aortic atherosclerosis. Cardiovascular disease (CVD) remains among the top 2 causes of death in the United States since 1975 with 633,842 deaths or 1 in 4 deaths, heart disease was the leading cause of death in 2015 followed by 595,930 cancerrelated deaths. Although the age-adjusted rate and acute mortality from myocardial infarction have decreased over time, reflecting progress in diagnosis and treatment over the past two decades, the risk of heart disease remains high with an estimated risk of 50% at 45 years in general. Therefore, one of the diagnostic and therapeutic methods that is currently having the greatest success is Cardiovascular Magnetic Resonance, as reported by the study carried out by Arun et al, in which they identify on the SCMR (Society for Cardiovascular Magnetic Resonance), a case series designed to present case reports demonstrating the unique attributes of Cardiovascular Magnetic Resonance in the diagnosis or treatment of cardiovascular disease, in order to avoid invasive studies or procedures, as well as cardiac biopsy and other procedures [27]. Another study carried out by Marianna et al, in which they report a clinical case of an underdiagnosed and underestimated disease of heart failure, cardiac amyloidosis. Presents the case of a 77-yearold man who presented with dyspnoea and weight loss. Endoscopy and duodenal biopsy showed amyloid deposits, subtyped as transthyretin type, EKG showed atrial fibrillation and moderate increase in wall thickness with moderate to severe diastolic dysfunction on echocardiography. Cine Cardiovascular Magnetic Resonance images supported the echocardiographic and gamma graphic findings. Tissue characterization showed clear amyloidosis with elevated native myocardial T1. Demonstrating the utility of Magnetic Resonance [28]. These studies demonstrate the great diagnostic and therapeutic utility of Magnetic Resonance in heart disease, both in underdiagnosed and frequently diagnosed ones. A strength of the current study is the methodology implemented, regarding the literature search, and steps in the selection of relevant articles, quality assessment, and data extraction. However, this study has several limitations, which should be taken into account before reaching a conclusion, among these are the few studies analysing clinical trials of the great therapeutic utility that MRI could have both in the child population, paediatric and adult, so more studies are needed to answer these questions.
CONCLUSION
One of the main research tools that present greater clinical application in a safe and complete way is magnetic resonance imaging. It is one of the most accurate tools to quantify ventricular volume, function, and mass in both congenital and acquired heart disease. The main indications for MRI are evaluation of left and right ventricular volumes and mass, as well as systolic function, evaluation of congenital hereditary disease with shunt calculus, evaluation of myocardial viability, evaluation of pericardial disease, aortic disease, cardiac masses, non-ischemic cardiomyopathies, and myocardial perfusion. It has important applications in acute myocardial infarction, dilated cardiomyopathy, hypertrophic and arrhythmogenic right ventricular cardiomyopathy, among other heart diseases. In this study we can identify the great therapeutic and diagnostic importance of cardiovascular Magnetic Resonance, and its great impact that it could have in the clinic of all patients with heart disease, in order to provide timely management depending on the ethology and pathology.
REFERENCES
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, et al. (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8): 891-975.
- Carvalho-Pinto BP, Faria CD (2016) Health, function and disability in stroke patients in the community. Braz J Phys Ther 20(4): 355-366.
- Harris C, Croce B, Cao C (2016). Thoracic aortic aneurysm. Ann Cardiothorac Surg 5(4): 407.
- Robson J, Ayerbe L, Mathur R, Addo J, Wragg A (2015) Clinical value of chest pain presentation and prodromes on the assessment of cardiovascular disease: a cohort study. BMJ Open 5(4): e007251.
- Khafaji HA, Suwaidi JM (2014) Atypical presentation of acute and chronic coronary artery disease in diabetics. World J Cardiol 6(8): 802-813.
- Khafaji HA, Suwaidi JM (2014) Atypical presentation of acute and chronic coronary artery disease in diabetics. World J Cardiol 6(8): 802-813.
- Trepanowski JF, Ioannidis JPA (2018) Limiting dependence on nonrandomized studies and improving randomized trials in human nutrition research: why and how. Adv Nutr 9(4): 367-377.
- Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, et al. (2014) 2019 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 140(11): e596-e646.
- Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. (2018) Risk assessment for cardiovascular disease with non-traditional risk factors: US preventive services task force recommendation statement. JAMA 320(3): 272-280.
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, et al. (2018) American heart association council on epidemiology and prevention statistics committee and stroke statistics subcommittee. Heart disease and stroke statistics-2018 update: a report from the American heart association. Circulation 143(8): e254-e743.
- Makowski MR, Henningsson M, Spuentrup E, Kim WY, Maintz D, et al. (2013) Characterization of coronary atherosclerosis by magnetic resonance imaging. Circulation 128(11): 1244-1255.
- Stacey RB, Hundley WG (2013) The role of cardiovascular magnetic resonance (CMR) and computed tomography (CCT) in facilitating heart failure management. Curr Treat Options Cardiovas 15(4): 373-386.
- Jahnke C, Manka R, Kozerke S, Schnackenburg B, Gebker R, et al. (2014) Cardiovascular magnetic resonance profiling of coronary atherosclerosis: vessel wall remodelling and related myocardial blood flow alterations. Eur Heart J Cardiovasc Imaging 15: 1400-1410.
- Abd‐Elmoniem KZ, Ramos N, Yazdani SK, Ghanem AM, Holland, et al. (2017) Coronary atherosclerosis and dilation in hyper IgE syndrome patients: depiction by magnetic resonance vessel wall imaging and pathological correlation. Atherosclerosis 258: 20-25.
- Asaumi Y, Noguchi T, Morita Y, Fujiwara R, Kanaya T, et al. (2015) Highintensity plaques on noncontrast T1‐weighted imaging as a predictor of periprocedural myocardial injury. JACC Cardiovasc Imaging 8: 741-743.
- Rommel KP, von Roeder M, Latuscynski K, Oberueck C, Blazek S, et al. (2016) Extracellular volume fraction for characterization of patients with heart failure and preserved ejection fraction. J Am Coll Cardiol 67(15): 1815-1825.
- Dusch MN, Thadani SR, Dhillon GS, Hope MD (2014) Diastolic function assessed by cardiac MRI using longitudinal left ventricular fractional shortening. Clin Imaging 38(5): 666-668.
- Bohnen S, Radunski UK, Lund GK, Kandolf R, Stehning C,et al .(2015). Performance of T1 and T2 mapping cardiovascular magnetic resonance to detect active myocarditis in patients with recent‐onset heart failure. Circ Cardiovasc Imaging 8: e003073.
- Yonezawa M, Nagata M, Kitagawa K, Kato S, Yoon Y, et al. (2014) Quantitative analysis of 1.5‐T whole‐heart coronary MR angiograms obtained with 32‐channel cardiac coils: a comparison with conventional quantitative coronary angiography. Radiology 271(2): 356-364.
- Townsend N, Nichols M, Scarborough P, Rayner M (2015) Cardiovascular disease in Europe-epidemiological update 2015. Eur Heart J 36(40): 2696-2705.
- Ehara S, Matsumoto K, Shimada K (2016) The clinical value of highintensity signals on the coronary atherosclerotic plaques: noncontrast T1‐weighted magnetic resonance imaging. Int J Mol Sci 17(7): 1187.
- Dweck MR, Williams MC, Moss AJ, Newby DE, Fayad ZA (2016) Computed tomography and cardiac magnetic resonance in ischemic heart disease. J Am Coll Cardiol 68(20): 2201-2216.
- Lota AS, Gatehouse PD, Mohiaddin RH (2017) T2 mapping and T2 imaging in heart failure. Heart Fail Rev 22(4): 431-440.
- Greenwood JP, Herzog BA, Brown JM, Everett CC, Plein S (2016) Cardiovascular magnetic resonance and single‐photon emission computed tomography in suspected coronary heart disease. Ann Intern Med 379(9814): 830-831.
- Mortality GBD Causes of Death C (2016) Global, regional, and national life expectancy, all‐cause mortality, and cause‐specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053): 1459-1544.
- Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, et al. (2015) Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 132(17): 1667-1678.
- Dahiya A, Chao C, Younger J, Kar J, Baldwin B, et al. (2021) Society for cardiovascular magnetic resonance 2019 case of the week series. J Cardiovasc Magn Reson 23(1): 44.
- Fontana M, Treibel A, Martinez A, Rosmini S, Kwong R (2017) A case report in cardiovascular magnetic resonance: the contrast agent matters in amyloid. BMC Med Imaging 17(1): 3.
Article Type
Research Article
Publication history
Received Date: December 06, 2022
Published: March 06, 2023
Address for correspondence
Jefferson David Jaimes Bautista, General physician, Universidad Industrial de Santander, Colombia; https://orcid.org/0000-0001-5042- 9663
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Jefferson David JB, Diana Marcela HM, Juan Pablo GM, Geinni Paola BA, Ingrid Tatiana PD, et. al. Role of Magnetic Resonance Imaging in the Diagnosis and Prognosis of Cardiomyopathy. 2023- 5(2) OAJBS.ID.000553.