Relationship of Liver Enzyme Levels with the Clinical Course of Covid-19
ABSTRACT
Introduction: SARS-CoV-2 / COVID-19 infection, which can affect many systems in the human body, can cause organ dysfunction.
High liver serum enzymes can be found in COVID-19 patients, and many factors cause this stop. Patients with high levels of liver
enzymes that require invasive mechanical ventilation during their follow-up were examined, and it was aimed to determine whether
it was among the predictive indicators of mortality.
Materials and Methods: Patients infected with COVID-19 who were hospitalized in the intensive care unit between March 30
and December 1, 2020 according to the criteria of hospitalization in the intensive care unit, clinical trials such as age, gender, length
of stay, additional diseases, liver enzyme levels and whether invasive mechanical ventilation is required their characteristics were
recorded and analyzed retrospectively and compared.
Results: Data were collected from 111 patients whose liver enzyme levels were measured from 131 patients included in the
study. It was found that aspartate transaminase, alanine aminotransferase, and gamma-glutamyl transferase levels were statistically
higher in the invasive mechanical ventilation group compared to the patients who did not undergo invasive mechanical ventilation.
Conclusion: Alanine aminotransferase, aspartate aminotransferase, and gamma-glutamyl transferase levels were statistically
higher in COVID19-infected patients who were treated in intensive care and undergoing invasive mechanical ventilation. These
enzymes are easily accessible and are shown among predictive values in mortality.
KEYWORDS
Covid-19; Mortality; Liver enzyme levels
INTRODUCTION
SARS-CoV-2 / COVID-19 infection has been spreading globally and threatening human health since the day it emerged. This epidemic, which emerged in China, spread throughout the world in a short time and affected millions of people [1]. COVID-19 infection infects many systems in the human body and causes organ dysfunction. It causes respiratory distress, especially with pneumonia, and affects the circulatory, hepatic, renal, and hematological systems [2,3]. High liver tests can be found in COVID-19 diseases, and the cause is unclear. It is thought that it may develop due to direct pathogenic effects of the SARS-CoV-2/COVID-19 virus, side effects of drugs used in moderate and severe COVID-19 patients, systemic inflammatory response, or hypoxia. However, there is uncertainty as to whether this elevation in liver enzymes increases the severity of the disease [4]. Some previous studies on SARS coronavirus have shown that liver enzymes may be elevated in patients infected with SARS [5]. In another study, it was thought that liver enzyme levels such as aspartate aminotranferase (AST) and alanin aminotransferase (ALT) were elevated in patients with COVID-19, and this infection could lead to liver damage [6]. Our aim is to examine the laboratory results of patients infected with COVID-19 in our hospital’s anesthesia intensive care units. To determine whether liver enzymes are among the predictive factors effective in showing the severity of the disease and mortality and to contribute to the literature on this subject. For this purpose, we grouped and examined patients according to their status of receiving invasive mechanical ventilation ( IMV) support, considering that the need for IMV support indicates that the disease is more severe.
MATERIALS AND METHODS
After the ethics committee approval was obtained between 30 March and 1 December, a total of 131 patients hospitalized in anesthesia intensive care units of our hospital due to covid19 were retrospectively reviewed. Patients with chronic liver disease and lack of data were excluded, and a total of 111 patients were included in the study. After obtaining ethics committee approval for this observational retrospective study, we reviewed the medical records of patients who were followed up and treated in anesthesia intensive care units due to COVID-19. After the patients were taken to the intensive care unit, clinical and biochemical data were collected retrospectively from medical records. The patients who did not receive IMV support were classified as Group 1, and the patients who were administered Group 2.
Inclusion Criteria
A radiologist confirmed patients aged 18 years and over who admitted to our hospital with complaints such as fever, cough, and shortness of breath, and after the diagnostic imaging findings of COVID-19 infection, the diagnosis of covid-19 was supported by the detection of nucleic acid in the respiratory tract by a polymerase chain reaction and met the criteria for admission to intensive care.
Exclusion Criteria from the Study
Patients with chronic heart disease, chronic alcohol use, and lack of data were excluded from the study.
Criteria for Admission to Intensive Care
Respiratory rate above 20 and oxygen saturation of 90 and below despite 100% oxygen support of 5lt/min with a reservoir oxygen mask or invasive mechanical ventilation support was applied to emergency departments with respiratory distress.
Invasive Mechanical Ventilation Application Criteria
In spite of HFNO or CPAP support, he was taken to invasive mechanical ventilation support in cases with oxygen saturation below 90%, respiratory rate above 2020, and deterioration of the patient’s hemodynamic findings.
STATISTICAL ANALYSIS
SPSS v20 program was used in the analysis of the data. Categorical variables were presented as number and percentage, numerical variables as mean and standard deviation. The distribution of categorical variables between groups was analyzed with the KI-Square test. The compatibility of numerical variables to normal distribution was investigated by the kolmogrofsimirnov test and graphing method. Mann Whitney-U was used for comparisons of numerical variables that were not normally distributed, and t-test was used for data that fit normal distribution and were homogeneous. P<0.05 was considered statistically significant. Pearson correlation analysis was conducted to examine the correlation of the data.
RESULTS
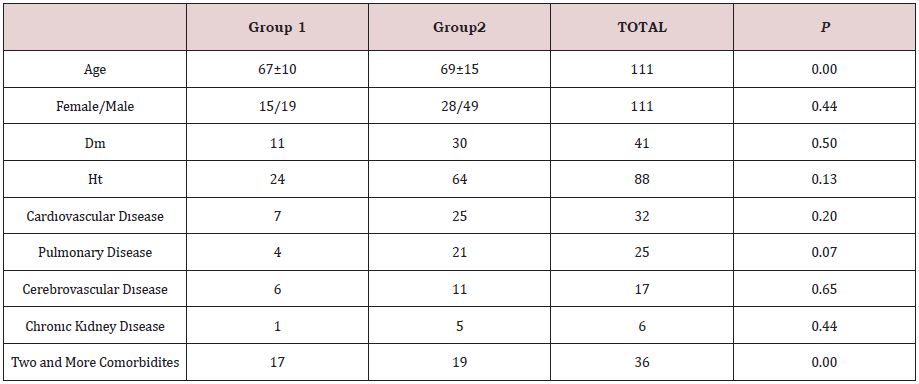
There were 34 patients in group 1 and 77 patients in group 2. 15 (%) of the patients in Group 1 and 28 of the patients in Group 2 were women. The mean age of the patients in Group 1 was 67±10, while the mean age of the patients in Group 2 was 69±15 (p: 0.00) (Table 1).
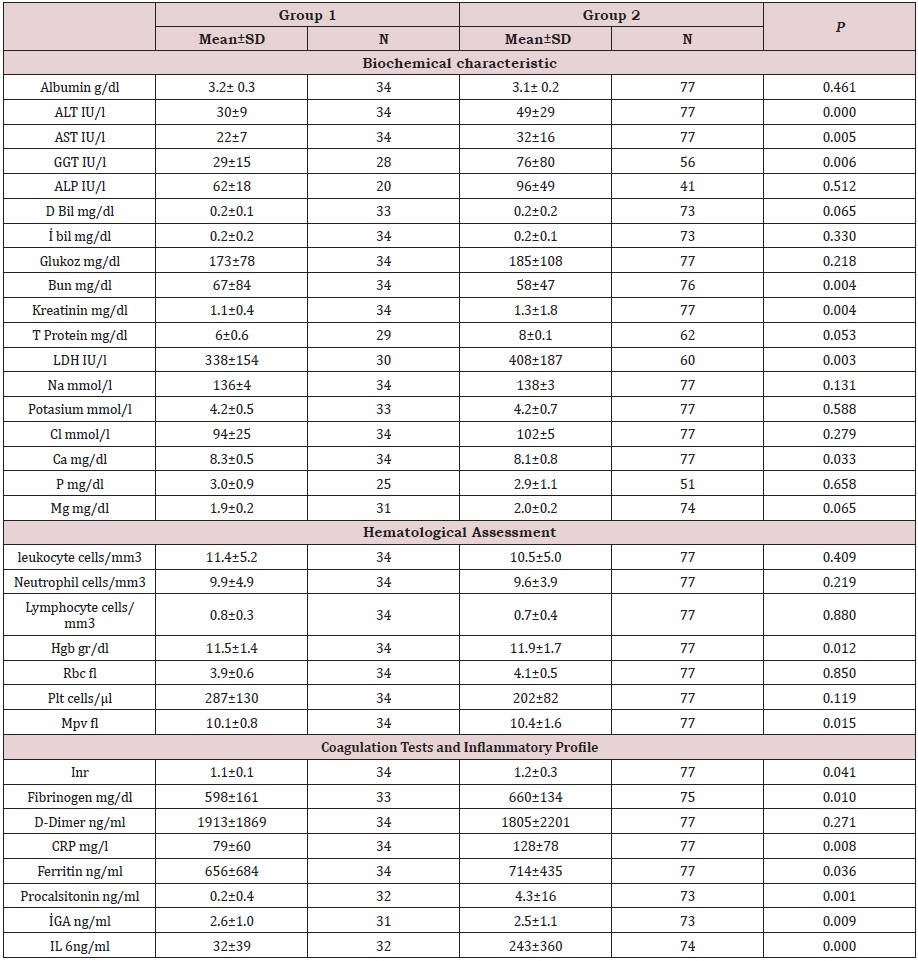
It was observed that 5 of 77 patients in Group 2 were admitted to the intensive care unit while under invasive mechanical ventilation support. It was observed that the other 72 patients received invasive mechanical ventilation support during their follow-up in the intensive care unit. While all 34 patients in Group 1 were discharged from the intensive care unit, only 4 of the errors in Group 2 were discharged from the intensive care unit (p: 0.00). ALT, AST, GGT and LDH were significantly higher in Group 2 than in Group 1. Respectively; (p: 0.000), (p: 0.005), (p: 0.006), (p: 0.003), (Table 2).
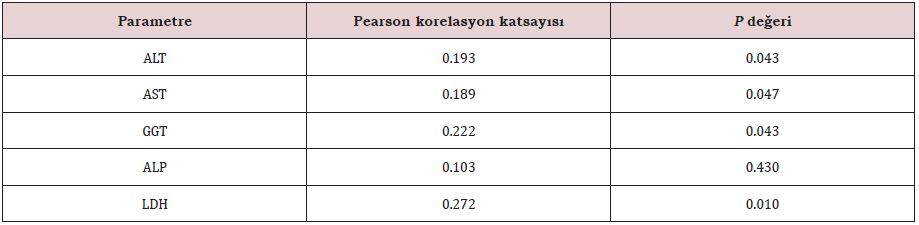
A positive correlation was found between ALT, AST, GGT and LDH levels and IMV support. Respectively; (p: 0.043, r: 0.193), (p: 0.047, r: 0.189), (p: 0.043, r: 0.222) (p: 0.010, r: 0.272), (Table 3).
Creatinine (p: 0.042, r: 193), sodium (p: 0.40, r: 195), chlorine (p: 0.44, r: 191), fibrinogen (p: 0.10, r: 247), A positive correlation was found between CRP (p: 0.006 r: 257), age (p: 0.10 r: 243) and IMV support. There was no correlation between other parameters and IMV support.
DISCUSSION
Due to the constantly increasing number of cases and deaths, it is important to understand the factors associated with mortality from covid 19 infection and the prognosis of this disease. Factors associated with mortality, especially in critical covid 19 patients hospitalized in intensive care units, include age, gender, and the presence of comorbid diseases [7]. In their study, guan et al. showed an increase in the need for invasive mechanical ventilation (IMV). In our study, when gender and diabetes mellitus, hypertension, chronic cardiological neurological, kidney, and lung disease were compared between the groups, there was no statistically significant difference. However, age and the presence of two or more diseases in group 2 were statistically higher than in group 1.
Covid 19 diseases are associated with elevated transaminases, d dimer, procalcitonin, and some laboratory findings such as troponin [8]. Some previous studies on sars coronavirus have shown that 34 % of patients infected with sars may have elevated liver enzymes. N protein and RNA polymerase gene fragments of the SARS virus were detected in hepatocytes in these patients. Covid 19 infection is thought to cause cellular damage and systemic inflammatory response by binding to ACE 2 receptors in the liver [9]. This binding is made through S proteins on the surface of the virus. It is thought that S2 protein is responsible for fusion while attaching to cells with S1 protein [10] that elevated liver enzyme levels such as AST and ALT can be seen in patients with covid 19, and the appearance of microvesicular steatosis and mild lobularity in the liver in autopsies of some covid 19 patients suggests that liver damage may be caused by this infection [6]. It has been shown that Sars Cov-2 infection is a disease that causes coagulopathy and thrombosis and can cause tissue edema and damage due to diffuse coagulation. Hepatic ischemic perfusion injury is thought to cause inflammation and cell damage by activating Kupfer cells, neutrophils, and platelets [1-11]. Tijera et al. In their study, it was observed that significant increases in liver enzymes play a very important role in the more severe course of COVID-19 [12]. Similarly, some studies have reported higher mortality in COVID-19 patients with elevated liver enzymes [13-17]. The mortality rate was 88-97% in covid 19 patients who received IMV support [18-19].
In our study, serum liver enzyme levels were found to be statistically higher in GROUP 2. In addition, a positive correlation was found between AST, ALT, LDH and GGT, and IMV support. This situation can be accepted as an early predictive indicator of mortality and the need for mechanical ventilation in patients with high transaminase levels.
It is thought that direct pathogenic effects of the virus, side effects of drugs used in critically ill patients, chronic hypoxia, and systemic inflammatory response may play a role as the cause of elevated serum transaminase levels in patients with Covid 19 [4].
All of the patients included in our study were critical covid 19 patients who were initiated antiviral therapy and were taken to intensive care due to respiratory distress and hypoxia. The antiviral and antibiotic drug groups used and hypoxia may have caused elevated liver enzyme levels.
CRP, Ferritin, IL-6, and procalcitonin levels are also parameters considered as indicators of mortality in Covid 19 patients [20]. In our study, inflammatory cytokines and procalcitonin levels such as CRP procalcitonin and IL-6 were also found to be statistically higher in the group patients who needed IMV support compared to the patients who did not, and this supports that systemic inflammatory response may be more severe. However, the measurement of transaminases is more practical and applicable; It is more useful alongside other parameters that are limited in use.
CONCLUSION
There are many factors related to morality in critical covid 19 patients. During the Kovid 19 pandemic, the need for MV and intensive care beds has increased all over the world. It is important to predict the severity of the disease in advance in terms of early preparation and planning of treatment by anticipating the need for mv and intensive care beds. Measurement of liver enzymes is an easy and inexpensive method that can be applied in many centers. In our study, we found that the disease was more severe in patients with high kc enzymes. Elevation of liver enzymes may be one of the predictive factors in showing the severity of covid 19 diseases. More studies are needed.
REFERENCES
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708-1720.
- Huang C, Wang Y, Li X, Lili R, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 395(10223): 497-506.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novelcoronaviruspneumonia in Wuhan, China: A descriptive study. Lancet (London, England) 395(10223): 507-513.
- Ali N, Hossain K (2020) Liver injury in severe COVID-19 infection: Current insights and challenges. Expert Rev Gastroenterol Hepatol 14(10): 879-884.
- Hao SR, Zhang SY, Lian JS, Xi J, Cheng Y, et al. (2020) Liver enzyme elevation in coronavirus disease 2019: A multicenter, retrospective, cross-sectional study. Am J Gastroenterol 115(7): 1075-1083.
- Cai Q, Huang D, Yu H, Zhu Z, Xia Z, et al. (2020) COVID-19: Abnormal liver function tests. Journal of Hepatology 73(3): 566-574.
- Orwa A, Rama B, Jer PO, Siti M, Sheikh G (2020) Risk factors for mortality among COVID-19 patients. Diabetes Research and Clinical Practice 166: 108293.
- Lippi G, Plebani M (2020) Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med 58(7): 1131-1134.
- Chai X, Hu L, Zhang Y, Han W, Lu Z, et al. (2020) Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. bioRxiv.
- Zhong P, Xu J, Yang D, Shen Y, Wang L, et al. (2020) COVID-19-associated gastrointestinal and liver injury: Clinical features and potential mechanisms. Signal Transduct Target Ther 5(1): 256.
- Varga Z, Andreas JF, Peter S, Martina H, Rea A, et al. (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395: 1417-1418.
- Higuera-de TF, Servín CA, Reyes HD, Argelia FL, Enrique JR, et al. (2021) Impact of liver enzymes on SARS-CoV-2 infection and the severity of clinical course of COVID-19. Liver Res 5(1): 21-27.
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. (2020) Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395: 1054-1062.
- Yang F, Shi S, Zhu J, Shi J, Dai K, et al. (2020) Analysis of 92 deceased patients with COVID-19. J Med Virol 92(11): 2511-2515.
- Mao R, Qiu Y, He JS, Tan JY, Li XH, et al. (2020) Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: A systematic review and meta-analysis. Lancet Gastroenterol Hepatol 5: 667-678.
- Cao J, Tu WJ, Cheng W, Yu L, Liu YK, et al. (2020) Clinical features and short-term outcomes of 102 patients with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis 71: 748-755.
- Chen R, Liang W, Jiang M, Guan W, Chen Z, et al. (2020) Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest 158(1): 97-105.
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. (2020) Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395(10229): 1054-1062.
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, et al. (2020) Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 323(20): 2052-2059.
- Pozzobon FM, Perazzo H, Bozza FA, Rodrigues RS, de Mello PR, et al. (2021) Liver injury predicts overall mortality in severe COVID-19: A prospective multicenter study in Brazil. Hepatol Int 15(2): 493-501.
Article Type
Research Article
Publication history
Received Date: December13, 2022
Published: February 04, 2022
Address for correspondence
Harun Tolga Duran, Anesthesiology and Reanimation Department, Ünye State Hospital, Turkey
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Ulku İ, Harun TD. Relationship of Liver Enzyme Levels with the Clinical Course of Covid-19. 2022- 4(1) OAJBS.ID.000391.