Pulmonary Ultrasound vs Radiography as a Diagnostic Method of Pneumonia in Pediatric Patients
ABSTRACT
Introduction: Pneumonia is an inflammation of the pulmonary parenchyma mainly due to an infectious process, Acute lower
respiratory tract infections represent one of the main causes of morbidity and mortality in the pediatric population worldwide,
so their diagnosis is of great importance for the treatment of patients; In recent years, there has been increasing evidence of the
usefulness of ultrasound and chest radiography in the management of patients with pulmonary processes, among which pneumonia
stands out.
Methodology: A bibliographic search was carried out in databases, selecting original articles, case reports and bibliographic
reviews from 2013 to 2021, using the documents that will treat Lung ultrasound vs radiography as a diagnostic method for
pneumonia in pediatric patients, obtaining 21 articles for the realization of this document.
Results: In 2012, a total of 102 patients with clinical suspicion of pneumonia were studied [14]; RT and EP were performed
on the same day. Conducted a randomized study of diagnostic tests comparing PE and RT in patients admitted to their emergency
department with a clinical suspicion of pneumonia, including a total of 191 patients aged from 0 months to 21 years of age [17].
Conclusion: Lung ultrasound has better sensitivity and specificity than chest X-ray.
KEYWORDS
Pneumonia; Chest x-ray; Ultrasound; Paediatric patients; Diagnostic tests
ABBREVATIONS
BTS: British Thoracic Society; RT: Reference Standard; CAP: Community Acquired Pneumonia; PUS: Pulmonary Ultrasound; SNP: Severe Neonatal Pneumonia; NICU: Neonatal Intensive Care Unit
INTRODUCTION
Pneumonia is the presentation of an infectious process that compromises the parenchyma of the lungs, under a histological diagnosis. Clinically we can recognize it as the acute presence of an increase in temperature (fever) and respiratory symptoms that may or may not be accompanied by radiographic findings of pulmonary parenchymal infiltrates [1,2]. Acute lower respiratory tract infections represent one of the main causes of morbidity and mortality in the pediatric population worldwide. Despite the great reduction in infant mortality in the first decade of this century, it remains high in developing countries, and represents up to 15% of total global mortality [1]. In 2015, there were an estimated 200 million cases of pneumonia in children under 5 years of age, of which about 15 million progressed to severe clinical forms and have caused 2 million deaths. The incidence and mortality from pneumonia has an inverse relationship with age in Pediatrics. The greatest burden of this disease is represented in the smallest, mainly those under 2 years of age, where pneumonia has partial mortality rates for this cause of up to 80%. 70% of mortality from pneumonia in children under 5 years of age occurs in developing countries [3].
Viruses are responsible for most cases of pneumonia in children, mainly in those under 2 years of age, with a global prevalence of 14-62%, reaching 40% in those under 6 months of age and 30% between 6 months and 2 years. Streptococcus pneumoniae is the most frequent germ in bacterial pneumonia; it affects 0.7 to 1 million children under 5 years of age who live in developing countries [4,5]. Clinical ultrasound is an ultrasound-based technique that is performed at the patient’s bedside, integrating ultrasound findings with clinical information and physical examination in real time. Its objective is to answer a specific question, and it provides information that allows guiding the diagnosis or the initial therapeutic attitude in a short time [1,2]. Due to the fact that it is a non-invasive and innocuous technique, its use in Pediatrics has increased notably in recent years, especially in the emergency and intensive care areas.
In recent years, there has been increasing evidence of the usefulness of ultrasound in the management of patients with pulmonary processes, among which pneumonia stands out. Thoracic ultrasound does not expose the child to ionizing radiation, when a specific diagnostic approach is required, obtaining skills is quick for the provider, and it can also be performed practically anywhere in a hospital center, without the need to move the patient [6,7]. Several studies have described the value of lung ultrasound in specific clinical situations compared to conventional chest imaging modalities such as chest radiographs and computed tomography [8]. However, its use is not yet routine in emergency rooms and hospitalizations, thoracic ultrasound is left for clinical indications that include, among others, dyspnea, respiratory failure, shock in any of its types, clinical pneumothorax, evaluation of pleural effusions, evaluation of the presence of alveolar consolidation, diaphragmatic function, trauma, intrathoracic masses, as well as planning and orientation for an invasive thoracic procedure [9]. The guidelines recommend not using routine chest radiographs to confirm suspected community-acquired pneumonia in children not requiring hospitalization and suggest monitoring the clinical course of patients [10]. Chest radiography at an official British Thoracic Society (BTS) audit identified that a chest radiography had been performed to confirm the diagnosis in 90% to 94% of suspected cases of community-acquired pneumonia and concluded that there was an excess Trusted in investigations to diagnose pneumonia [11].
METHODOLOGY
To carry out this article, a bibliographic search was carried out in various databases such as Elsevier, Scielo, Medline, pubmed, ScienceDirect and Ovid, thus selecting original articles, case reports and bibliographic reviews from 2013 to 2021, in Spanish and English. using MeSH terms: Pneumonia, chest x-ray, ultrasound, pediatric patients, diagnostic tests, and the Boolean operators and or. Thus, including all the documents that will deal with lung ultrasound vs radiography as a diagnostic method for pneumonia in pediatric patients, the data found were 30 records, thus using 21 articles for the preparation of this document.
RESULTS
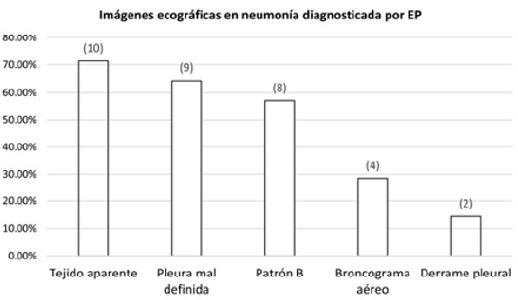
In a single-center prospective observational study, carried out in the Pediatric Emergency Department of the Parc Taulí University Hospital in Sabadell between November 2015 and May 2017, patients under 18 years of age with suspected pneumonia were included, defined as patients with respiratory symptoms more at least one of the following symptoms: fever greater than 38 °C of more than 48 h of evolution, altered general appearance or suggestive auscultation (crackles, tubal murmur, hypophonesis). And they excluded patients with underlying lung disease (cystic fibrosis, lung transplant, bronchopulmonary dysplasia, post-thoracic surgery). The most frequent ultrasound images in pneumonia diagnosed by PE were apparent tissue image in 10 cases (71.4%), poorly defined pleura in 9 (64.3%), underlying pattern B in 8 (57.1%), air bronchogram in 4 (28.6%) and pleural effusion in 2 (14.3%) Of the 2 pleural effusions detected by PE, 1 was not detected by RT (parapneumonic effusion <1 cm that resolved with intravenous antibiotic treatment) The mean time needed was 9 min (SD 3.5) for EP and 25 min (SD 9.2) for RT, with a difference of 16.2 min (95% CI: 12.7-19, 6), p < 0.01. (Figure 1) [12].
[13] carried out a meta-analysis in 2015 in which a systematic search was carried out in different databases where they compared EP diagnostic accuracy against a reference standard (RT). As a result, eight studies (765 children) were reviewed for analysis, of which 6 were conducted in the general pediatric population and 2 in neonates. Five studies (63%) reported the use of highly skilled sonographers. PE had a sensitivity of 96% (95% CI 94-97%) and a specificity of 93% (95% CI 90-96%), and the positive and negative odds ratios were 15.3 (95% CI 6.6-35.3). and 0.06 (95% CI 0.03- 0.11), respectively.
[14] In 2012, a total of 102 patients with clinical suspicion of pneumonia were studied; RT and EP were performed on the same day. As a result, a total of 89 patients had the diagnosis of Community Acquired Pneumonia (CAP) confirmed, of which the pulmonary ultrasound yielded a total result of 88 patients, while the chest X-ray a total of 81 patients; furthermore, lung ultrasound was able to identify pleural effusion in 16 cases, while RT only detected 3 cases. luri, de Candia and pazzochi conducted a study in Italy in 2009 in 28 patients aged between 4 months and 17 years with clinical suspicion of community-acquired pneumonia (CAP), comparing RT and PE as a tool diagnostic. In the results of the RT, subpleural consolidations were identified in 22 of the patients, 7 perihilar consolidations, and 8 pleural effusions, while the EP found the same 22 subpleural consolidations, but did not identify any perihilar consolidation, however, it was detected. a total of 15 pleural effusions, thus achieving a sensitivity of 91.67% and a specificity of 100% [15].
[16] carried out a study that included a total population of 103 patients where the EP was practiced by pediatric residents after receiving training in said imaging study and even so they report a sensitivity of 97.9% and a specificity of 94.5% of the EP for the diagnosis of CAP. Recently, [17] conducted a randomized study of diagnostic tests comparing PE and RT in patients admitted to their emergency department with a clinical suspicion of pneumonia, including a total of 191 patients aged from 0 months to 21 years of age. Those who practiced sonographer services were emergency department physicians who received 1 hour of training. These patients were randomly assigned to initially undergo PE or RT. Patients who were assigned to RT subsequently had to undergo EP, while those who initially underwent EP could undergo RT if the medical team or the patient’s family considered it necessary, however, it is not identified as mandatory. Of the 103 patients who started in the EP group, 61% subsequently underwent RT; Of these, in 29 cases (28%) they were requested from admission, by the family or by the doctor after performing the EP, and even so, none of the RTs showed results different from those of the EP. On the other hand, in neither of the 2 groups were CAP diagnoses missed [17].
In 2014 in Beijing, they carried out an observational study with the aim of investigating the findings of pulmonary ultrasound (PUS) in severe neonatal pneumonia (SNP) in order to assess its diagnostic capacity for this disease. 40 neonates diagnosed with NNS participated according to their medical history, including their clinical manifestations and chest X-ray findings suggestive of this, with the final participation of 40 neonates without lung disease who formed the control group, all of them admitted in the neonatal intensive care unit (NICU). They were excluded if there was no definitive evidence of infection or if they had serious complications that could affect the Echo findings, which was performed by a single investigator, unaware of the diagnosis. The main ultrasound findings in patients with NNS were, respectively: pulmonary consolidation and interstitial syndrome in 100%; pleural line abnormalities in 90%; disappearance of lung sliding in 75%; dynamic air bronchograms in 52.5%; pulmonary pulse in 30%; pleural effusion in 20%. The only finding found in the subjects belonging to the control group was some B lines in 30%. Thus, the value of p <0.001 the data obtained. Large areas of pulmonary consolidation with irregular margins demonstrated a sensitivity and specificity of 100% for the diagnosis of NNS. dynamic air bronchograms in 52.5%; pulmonary pulse in 30%; pleural effusion in 20%. The only finding found in the subjects belonging to the control group was some B lines in 30%. Thus, the value of p <0.001 the data obtained. Large areas of pulmonary consolidation with irregular margins demonstrated a sensitivity and specificity of 100% for the diagnosis of NNS. dynamic air bronchograms in 52.5%; pulmonary pulse in 30%; pleural effusion in 20%. The only finding found in the subjects belonging to the control group was some B lines in 30%. Thus, the value of p <0.001 the data obtained. Large areas of pulmonary consolidation with irregular margins demonstrated a sensitivity and specificity of 100% for the diagnosis of NNS [18].
DISCUSSION
In the study carried out by Gelman and collaborators, they included 37 patients, of which 17 of these were diagnosed with pneumonia, most of these were in a mean age of 3 years and likewise >50% were girls, of these 17 In 14 of them, the ultrasound was positive and in the remaining 3 the ultrasound was negative. The most common ultrasound images in the lung ultrasound diagnosis of pneumonia were images of evident tissue in 10 cases (71.4%), edge unclear pleural effusion in 9 cases (64.3%), latent type B in 8 cases (57.1%), bronchial air in 4 cases (28.6%) and pleural effusion (14.3%), likewise, PE is an excellent test for the diagnosis of pneumonia in childhood, based on the improvement of quality of care and patient safety, which is why the use of PE is recommended as a first-line test for the diagnosis of pneumonia in childhood. childhood, however, The results of this study support the usefulness of Echo P as the technique of choice for the diagnosis of pneumonia in children, with high precision, slightly higher than RT, and less time consumption, results consistent with the existing literature [19].
In pneumonia Due to its frequency in clinical practice without a doubt and frequently in children, chest ultrasound is most useful in Primary Care (if the lesion is > 1 cm, the changes are important, the clinical relevance of the lesions < 1 cm is not fully known). Dynamic, aerial or liquid bronchial images (according to evolution time) and dendritic, hepatic, and lamellar atelectasis. If it is not a large sheet, the edge is jagged. B lines appear behind the lesion. Fragmented and thickened pleural line Basal parapneumonic effusion. Doppler: increased vascularization [20]. According to a study carried out by Molina and Ortega, where eight studies with a total of 765 subjects were evaluated, the result was that ultrasound was shown to be useful and effective for the diagnosis of pneumonia, with an S of 96% (CI 95: 94 to 97), where for every eleven ultrasounds performed on these patients, ten of them were diagnosed with pneumonia; Although various studies conclude that there is not a high relevance between the use of ultrasound vs. chest X-ray and despite the heterogeneity in the studies and the skill of the sonographers, lung ultrasound is recommended and is a good tool for the diagnosis of lung cancer. pneumonia in pediatric patients and this can be considered a viable alternative for the timely diagnosis of pneumonia in children [21].
CONCLUSION
Among the imaging tests performed for the diagnosis of pneumonia in pediatric patients, we have, among others, lung ultrasound and chest radiography, where according to the results of multiple studies, ultrasound has better results in the diagnosis of pneumonia, showing high sensitivity and specificity, it was also better in the identification of pleural effusion in patients compared to chest radiography, because it manages to identify effusions when they are of greater content; However, the chest X-ray is a good diagnostic option for the identification of this pathology, as it has specific radiological signs of pneumonia, such as air bronchograms, which are of great help in the imaging diagnosis.
REFERENCES
- Messinger JA, Kupfer O, Hurst A, Parker S (2017) Management of pediatric community-acquired bacterial pneumonia. Pediatr Rev 38(9): 394-409.
- Prayle A, Atkinson M, Smyth A (2011) Pneumonia in the developed world. Pediatr Respir Rev 12(1): 60-69.
- Leung A, Wong A, Hon K (2018) Community-acquired pneumonia in children. Recent Pat Inflamm Allergy Drug Discov 12(2): 136-144.
- Reali F, Sferrazza Papa GF, Carlucci P, Fracasso P, Di Marco F, et al. (2014) Can lung ultrasound replace chest radiography for the diagnosis of pneumonia in hospitalized children. Respiration 88(2): 112-115.
- De La Rosa R, Redondo Y, Quintero G, Mendoza L, Salcedo J, et al. (2018) Pulmonary echography as a diagnostic tool of pneumonia acquired in the community in children. Revista Salud Uninorte 34(1): 174-184.
- Dominguez A, Gaspar HA, Preto M, Ejzenberg FE (2018) Point-of-care lung ultrasound in pediatric critical and emergency care. J Paediatr Child Health 54(9):945-952.
- Conlon TW, Nishisaki A, Singh Y, Bhombal S, De Luca D, et al. (2019) Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics 144(4): e20191402.
- Rambhia SH, D’Agostino CA, Noor A, Villani R, Naidich JJ, et al. (2017) Thoracic Ultrasound: Technique, Applications and Interpretation. Curr Probl Diagn Radiol 46(4): 305-316.
- Villa González JM (2021) Ecografía pulmonar clínica en el paciente pediátrico con sospecha de neumonía en urgencias: estudio de concordancia interobservador. eko apirilaren.
- Shaha N, Bachur R, Simel D, Neuman M (2017) Does this child have pneumonia? the rational clinical examination systemat ic review. JAMA 318(5): 462-471.
- Grarber M, Quinonez R (2018) Chest radiograph for childhood pneumonia: good, but not good enough. Pediatrics 142(3): e20182025.
- Gelman A, Valdovinos LR, Málaga AR, Olomí IB, Villanueva SM, et al. (2022) Usefulness and acceptance of lung ultrasound for the diagnosis of pneumonia in children. Medicina Clínica Práctica 5(2): 100279.
- Pereda M, Chavez M, Hooper-Miele C, Gilman R, Steinhoff M, et al. (2015) Lung ultrasound for the diagnosis of pneumonia in children: a metaanalysis. Pediatrics 135(4): 714-722.
- Caiulo VA, Gargani L, Caiulo S, Fisicaro A, Moramarco F, et al. (2013) Lung ultrasound characteristics of community acquired pneumonia in hospitalized children. Pediatr Pulmonol 48(3): 280-287.
- Luri D, De Candia A, Bazzocchi M (2009) Evaluation of the lung in children with suspected pneumonia: usefulness of ultrasonography. Radiol Med 114(2): 321-330.
- Esposito S, Papa SS, Borzani I, Pinzani R, Giannitto C, et al. (2014) Performance of lung ultrasonography in children with communityacquired pneumonia. Ital J Pediatr 40: 37.
- Jones B, Tay E, Elikashvili I, Sanders J, Paul AZ, et al. (2016) Feasibility and safety of substituting lung ultrasound for chest x-ray when diagnosing pneumonia in children: a randomized controlled trial. Chest 150(1): 131-138.
- Liu J, Liu F, Liu Y, Wang HW, Feng ZC (2014) Lung ultrasonography for the diagnosis of severe neonatal pneumonia. Chest 146(2): 383-388.
- Gelman A, Renter L, Renera A, Baena I, Moya S, et al. (2022) Usefulness and acceptance of lung ultrasound for the diagnosis of pneumonia in children. Medicina Clínic pediatric 5(2): 100279.
- Bilbao Sustacha JA, Peix Sambola MA, Alonso Martín DE, Díaz Lázaro J (2019) Aplicación de la ecografía clínica pediátrica en Atención Primaria. En: AEPap (Edn). Congreso de Actualización. Pediatría Madrid: Lúa Ediciones 3.0; 495-506.
- Molina AM, Ortega PE (2015) Lung ultrasound is useful for the diagnosis of pneumonia in children. Evid Pediatr 11: 60.
Article Type
Mini Review
Publication history
Received Date: August 25, 2022
Published: November 29, 2022
Address for correspondence
Jesús David GB, Universidad Libre, Colombia
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Jesús David GB, Jose Dario OG, Eduard Orlando VP, Zaira Molina A, Karen Dayana JH, Luis Miguel LM. Pulmonary Ultrasound vs Radiography as a Diagnostic Method of Pneumonia in Pediatric Patients. 2022- 4(6) OAJBS.ID.000521.