Myofibromatosis With Extension to The Submandibular Gland, Clinical Case Report
ABSTRACT
Myofibromatosis is a rare fibrous childhood tumor, with variable clinical behavior whose treatment is challenging in a country with scarce resources. The objective of this work is to report a clinical case of myofibromatosis in a child with the involvement of the right submandibular gland, whose treatment was surgical with satisfactory results, although periodic controls are mandatory due to the possibility of recurrences rarely described.
KEYWORDS
Myofibromatosis, Submandibular gland, Mozambique
INTRODUCTION
Rare, however, more common childhood disease, benign, with unknown pathogenesis [1-6]; myofibromatosis is defined as a mesenchymal disorder, is sporadic characterized by a fibrous proliferation of the skin, bone, muscle and viscera [5,7,8]. Sometimes it presents a volume increase that exhibits rapid growth [1]. According to the WHO, it is clinically classified as solitary, multicentric myofibromatosis without viscera involvement, and multicentric with viscera involvement (generalized) [2,9].
They show a predilection for the head and neck region, being the most common oral location the mandible, tongue and jugal mucosa, following the abdomen [2], when involving viscera, the most common are the cardiopulmonary system and digestive tract with higher morbidity and mortality [10]. Conservative management and controls are recommended for solitary or multicentric forms without visceral involvement, as spontaneous regression usually occurs [8,10].
Surgical treatment is recommended when these because mass effects [8]. Aggressive treatment with radiotherapy, chemotherapy and radical surgery is used for disseminated forms with visceral involvement [8]. The aim of this study is to report a clinical case of myofibromatosis in a child with involvement of the right submandibular gland, whose treatment was surgical with satisfactory results in a country with few resources.
CASE REPORT
A 23-month-old female child, melanoderme, transferred from Tete (Mozambique), with a history of disease evolution about 3 months, with progressive increase in volume in the submandibular region, rapidly growing, painless, without fever. He denies a history of illness and hospitalization. Denies family history of illness. Denies history of allergies (Figure 1).
On physical examination, a facial asymmetry was observed at the expense of a hard elastic mass fixed to the deep planes, located in the submandibular region to the right, crossing the midline, slightly painful palpation, no lesions at the skin level, without change in skin color (Figure 1). Intraoral inspection revealed intact mucosa with no signs of lesions, tongue motricity was maintained, without involvement of dental arches. Hemodynamically stable, with the remaining organs and systems without significant changes.
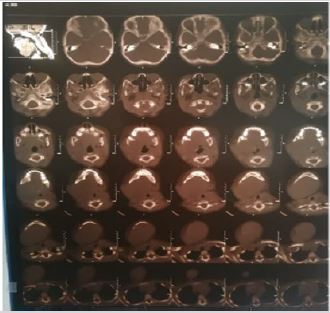
On the right submandibular ultrasonography, she presented normal thick skin. Large hypoeogenic lesions were observed in the submandibular region with poorly defined contours, with calcifications, of tumor aspect, impresses correspond with tumor lesion of the bone. Associated with lymphadenomegaly, dimensions of 15x12mm. Abdominal ultrasonography, within normal standards. CT scan reveals a large solid mass is observed, located in the right submandibular region of variable density (29-42HU) predominantly hyperdense in its interior, or areas of necrosis (in relation to the neoformative/tumor). It meets the base of the tongue, laterally meets the parotid, medially displacing the digastric and Hyoid muscle. There is also slight bone erosion of the right lateral phase of the mandibula. parapharyngeal spaces and unchanged pterygopalatine fossa. Preserved muscle and adipose planes (Figure 2).
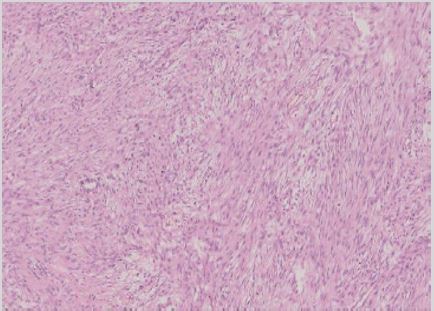
Routine blood tests (blood count and biochemistry) were within the parameters considered physiological, negative serology for HIV, an incisional biopsy was made, whose histological result was compatible with that of myofibromatosis (Figure 3), the patient was later prepared for surgical excision and submaxilectomy under general anesthesia (Figure 4 & 5).
Fragments are observed that show a lesion composed of bundles of fusiform cells with atypia that sometimes form a tourbillon, with lumen of vascular aspect. Low mitotic index without necrosis. Marginal excision.
Figure 3 Intraoperatively, excision of the mass “in totus” and submaxilectomy, where a well-circumscribed mass measuring more than 10X5cm was observed, removed from the submandibular region that caused minimal right mandibular bone erosion and patient on the sixth postoperative day, after removal of stitches, facial edema in gradual regression, with satisfactory evolution of the condition (Figure 4).
DISCUSSION
In 90% of the cases this tumor occurs in children under 2 years with a slight predilection for the male sex, in this case we describe this tumor in a 23 months old female patient, which supports the literature [5]. This tumor can classically present itself in solitary form, a single lesion that affects the skin and or muscles of the head, neck, or trunk in 75% of cases [1]. In the multicentric form involving skin, subcutaneous cellular tissue, muscle, and bone [5].
In the multicentric form with visceral involvement may involve cardiopulmonary system, thyroid gland, adrenal, kidneys, pancreas, and gastrointestinal tract and rarely the nervous system [2]. In this case, we describe the solitary form with involvement of the submandibular gland in which a sub-maxillectomy was mandated, a fact that according to the literature consulted describes to be very rare [2] and little is known about it.
Myofibromatosis treatment for solitary lesions consists of the excision of the mass, although the literature mentions that lesions of reduced size may resolve spontaneously [1,6], in this case despite the solitary form due to the effect of marked mass, the excision of the mass associated with submaxilectomy was made because it involves the submandibular gland. However, satisfactory results have been observed. Although rare, periodic clinical and radiographic controls will be mandated according to the literature, with the aim of monitoring possible recurrence [2,4,6,11]. There is no conclusive evidence to support the benefit of adjuvant radiotherapy or chemotherapy in solitary myofibromatosis [2].
CONCLUSION
Although benign, myofibromatosis may be aggressive with rapid growth, in which diagnosis and treatment should be instituted according to its presentation form. Although they are rarely recurrent, periodic controls are recommended.
REFERENCES
- Alexandra M, Benoit G, François T (2019) Infantile myofibromatosis treated by mandibulectomy and staged reconstruction with submental flap and free fibula flap: A case report. J Otolaryngol Head Neck Surg 48(1): 14.
- Bejjanki KM, Devjyoti T, Ruchi M (2019) Solitary orbital myofibroma in a child: A rare case report with literature review. Indian J Ophthalmol 67(7): 1240-1245.
- Bruna ELFM, Juliana SBO, Damião RFS (2012) Childhood myofibromatosis: Report of a rare disease. Radiol Bras 45(2): 118-120.
- Vieira F, Rocha YD (2015) Multifocal musculoskeletal myofibromatosis. An Pediatr (Barc) 83(1): 66-67.
- Margarita L, Bruno F, Juan PM, María AFB, José C, et al. (2017) Infantile myofibromatosis. An Bras Dermatol 92(6):854-857.
- Poflee SV, Bode AN, Chavarkar S, Umap PS (2017) Myofibromatosis: Utility of fine needle aspiration cytology in the diagnosis of an underreported entity. J Cytol 34(1): 53-55.
- Bencheikh R, Benhammou A, Mourtada F, Benbouzid MA, El Edghiri H, et al. (2007) Myofi bromatose infantile mandibulaire. La Lettre d’ORL et de chirurgie cervico-faciale 308: 22-24.
- Sergio S, Maria CT, Mario R, Maria P, Ottavio Z, et al. (2017) Wholebody magnetic resonance imaging in the diagnosis and follow-up of multicentric infantile myofibromatosis: A case report. Mol Clin Oncol 6(4): 579-582.
- Mohammed H, Erin B, Raphael W, Angshumoy R, Yanbin Z, et al. (2019) Novel PDGFRB rearrangement in multifocal infantile myofibromatosis is tumorigenic and sensitive to imatinib. Cold Spring Harb Mol Case Stud 5(5): a004440.
- Peter M, Ondrej S, Jakub N, Jana S, Kristyna M, et al. (2017) Case report: rapid and durable response to PDGFR targeted therapy in a child with refractory multiple infantile myofibromatosis and a heterozygous germline mutation of the PDGFRB gene. BMC Cancer 17(1): 119.
- Neville BW (2009) Patologia Oral e Maxilofacial, 3rd edn, pp.517- 518, Elsevier, Netherlands.
Article Type
Case Report
Publication history
Received date: June 25, 2020
Published date: July 27, 2020
Address for correspondence
Nadia AH Fortes, Department of Surgery, Oro- Maxillofacial Surgery Service, Maputo Central Hospital, Maputo-Mozambique
Copyright
©2020 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Nadia AHF, Jessica CdaC, Gizela M, Telmo M, Gonçalves U, Brian RJ, Bento M. Myofibromatosis With Extension to The Submandibular Gland, Clinical Case Report. 2020 - 2(4) OAJBS.ID.000198.