Lupus Nephritis: Viewing Kidneys Through Retinal Periscope
ABSTRACT
Hypertensive emergencies are rare in children and mostly attributable to some underlying disorder (secondary) rather than primary hypertension- renal disease being the most common cause. The child can have variable presentation depending on the target organ involved. Unlike benign hypertension, this requires simultaneous management and evaluation in a multidisciplinary approach. We report a case of a 16-year-old girl with complaints of acute onset blurring of vision and headache and diagnosed as Lupus nephritis presenting as hypertensive emergency. This case reiterates the importance of the extensive evaluation which is needed in such cases. Early intervention tends to drastically improve the clinical outcome, since such cases usually have a worse prognosis than their adult counterparts.
KEYWORDS
Chronic kidney disease; Hypertensive emergency; Hypertensive retinopathy; Lupus nephritis; SLE; Systemic lupus erythematosus
ABBREVATIONS
ANA: Anti-Nuclear Antibody; BP: Blood Pressure; CKD: Chronic Kidney Disease; DMSA: Dimercaptosuccinic Acid; Ds-DNA: Double Stranded- DNA; DTPA: Diethylenetriamine Pentaacetic Acid; ESRD: End Stage Renal Disease; LN: Lupus Nephritis; SLE: Systemic Lupus Erythematosus
INTRODUCTION
Hypertensive emergency is an acute medical condition, characterized by severely elevated blood pressure with end organ damage. Hypertension in children is usually secondary in nature, mostly due to renal diseases. It may manifest as hypertensive emergency or urgency, but most of the time, is detected incidentally. Lupus nephritis is a rare cause, mostly due to the lower prevalence of Systemic Lupus Erythematosus (SLE) in pediatric age group. Although the organ damage caused by hypertension is potentially reversible, it depends on the stage at which the treatment is instituted. Any potential delay in management adversely affects the outcome.
CASE PRESENTATION
Sixteen-year-old adolescent girl presented with complaints of progressive blurring of vision for one week. It was associated with frontal headache and intermittent episodes of blackouts. There was no history of decreased urine output/ swelling/ seizures/ focal deficits/ breathing difficulty/ joint pain/ oral ulcers.
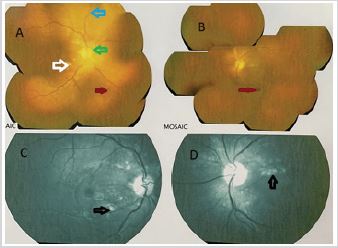
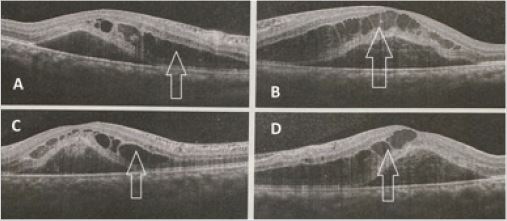
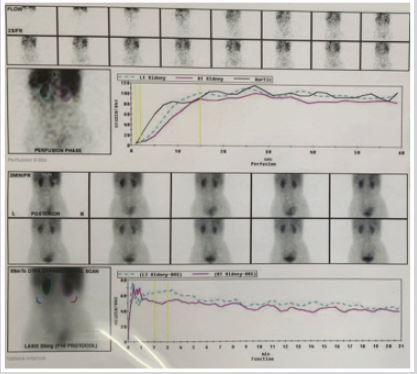
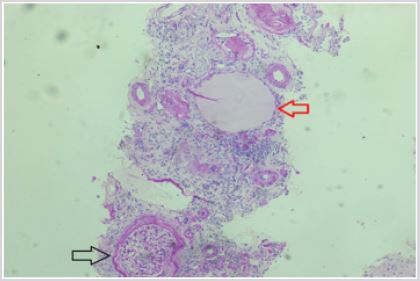
On examination, she had pallor, periorbital puffiness and alopecia with high blood pressures (BP) (BP: 182/140 mmHg), BP in all limbs being comparable. There were no focal neurological deficits/ signs of heart failure/bruit over renal arteries; with rest of systemic examination being normal. Fundoscopy revealed Grade IV hypertensive retinopathy (Figure 1 & 2). Investigations revealed normocytic normochromic anemia (Hemoglobin: 7.9g/ dL), deranged renal functions [Blood urea: 60 mg/dl; Serum creatinine: 3.7 mg/dl; estimated Glomerular Filtration Rate of 22.4 ml/min/1.73 m2] with hypocalcemia (8.1mg/dL) and proteinuria (~100mg/dL). Considering secondary causes for hypertension, further investigations were planned. Renal ultrasound showed small kidneys (right: 6.8cm x 2.75cm and left: 7.1cmx 3cm) with raised echogenicity and normal renal doppler, suggestive of chronic kidney disease (CKD). Further workup revealed low Vitamin D levels (72nmol/L) with raised Parathormone levels (1034.8pg/mL) and low Iron (34mcg/dL) and ferritin levels. Tc99m-dimercaptosuccinic acid (DMSA) and Diethylenetriamine pentaacetic acid (DTPA) scan showed globally impaired renal function (GFR: 25.87ml/min- left: 14.49ml/min and right: 11.39ml/min) with no scarring (Figure 3). Structural heart disease was ruled out by echocardiography. Etiological workup of CKD revealed normal C3 and C4 levels with negative anti Streptolysin-O titers and Direct Agglutination Test. Anti-Nuclear Antibody (ANA) was positive with mitosis positive centrosome and midbody pattern along with positive anti double stranded- DNA (ds-DNA) antibodies. Renal biopsy was suggestive of End Stage Renal Disease (ESRD) showing fibrosis with atrophic tubules (Figure 4-6). Hence, diagnosis of lupus nephritis was made. She was initially stabilized on IV labetalol and Mean Arterial Pressure reduction attained as per protocol. After initial stabilization, enalapril and later on amlodipine were added in view of persistent stage I hypertension. On follow up, visual acuity improved with no residual deficit along with control of BP. She is on renal replacement therapy and doing well on follow up.
DISCUSSION
Our index case presented with hypertensive emergency and was later diagnosed with lupus nephritis as the underlying etiology for End Stage Renal Disease. Renal diseases are the most common underlying cause of hypertension in children. Congenital anomalies of Kidney and Urinary tract is the most common etiology in children less than 12 years. Glomerular diseases are more common in children above 12 years of age [1]. Most of the cases are incidentally detected. It may also present as hypertensive urgency and emergency, manifesting as headache, visual changes, nausea, seizures, dizziness or epistaxis. It is characterized pathologically by increased intima-media thickness of arteries, left ventricle hypertrophy, increased arterial stiffness and glomerular and retinal changes [2]. Secondary hypertension has more propensity of developing into hypertensive crisis. Since most of the cases are asymptomatic and the prognosis is better when the disease is diagnosed early, it is prudent that all children above the age of three years should undergo an annual BP measurement [3]. Secondary hypertension evaluation is guided by the etiology specific to that particular age group and sex, like- renal parenchymal disease, endocrine causes, coarctation of aorta and essential hypertension. Careful clinical history is followed by baseline investigations including complete blood count, renal function tests and urine examination for proteinuria and hematuria (for glomerular involvement). Specific tests include vitamin D levels, parathormone and iron studies (chronic kidney disease), C3/C4 complements, Direct Agglutination Test, ANA and anti-dsDNA antibody titres for SLE, Anti-Nuclear Cytoplsmic Antibody (ANCA) for vasculitis, renal ultrasound-doppler to look for renal artery stenosis, and hormonal studies (endocrine causes). DMSA and DTPA scan are done for structural and functional assessment of kidneys.
Assessment for target organ damage includes an Electrocardiogram and Echocardiography to evaluate for left ventricular hypertrophy (LVH); and fundoscopy for hypertensive retinopathy [4]. LVH can occur in around 34% to 38% of the cases and mandates the intensification of therapy. Presence of retinopathy can be considered as a non- invasive marker of nephropathy [5]. Negative correlation between glomerular filtration rate (GFR) and retinopathy stage was also evident in our case.
Lupus nephritis is a rare cause of hypertensive emergency in children and is more severe than its adult counterpart [6]. Although it occurs in around 37-82% of children affected with SLE, the overall contribution is low due to less prevalence of SLE itself, the incidence of the same being 0.36-0.9/100,000 children/year [7]. To prevent rapidly evolving end-organ damage, patients with hypertensive emergency need prompt institution of BP reduction. IV labetalol is the most common first line therapy due to its efficacy and safety in children. Mean Arterial Pressure reduction should not exceed more than 25% over the first eight hours with complete normalization over next 24-48 hours. Rapid blood pressure reduction may lead to visual defects, renal insufficiency and permanent neurological sequelae.
Treatment of lupus nephritis (LN) consists of two phases: induction phase (three to six months) and maintenance phase (uptil three years). It predominantly depends on the stage of LN. Mycophenolate Mofetil (MMF) or cyclophosmamide is used for induction therapy. Hydroxychloroquine can also be used in such cases due to its potential benefit of reducing the renal damage. Immuno- globulin, plasma exchange or Rituximab may be used in refractory cases. Azathioprine, MMF or prednisolone may be used for maintenance therapy. Exacerbations are treated akin to first episode and in spite of early treatment, there is 10-20% chances for progression to ESRD. But if the diagnosis is delayed and lupus nephritis has progressed to ESRDas in our case, homeostasis cannot be maintained by medical therapy and may mandate hemodialysis or renal transplantation- the ultimate goal being the renal transplant for these patients after achieving immunological remission.
The presenting case reiterates the need for prompt evaluation and treatment in hypertensive emergency which is the key to prevent the irreversible damage in such cases. Considering multisystemic disease like SLE as the potential underlying etiology is of paramount importance which is often neglected in such cases with atypical presentation.
REFERENCES
- Kaspar CD, Bholah R, Bunchman TE (2016) A Review of pediatric chronic kidney disease. Blood Purif 41(1-3): 211-217.
- Patel N, Walker N (2016) Clinical assessment of hypertension in children. Clin Hypertens 22: 15.
- Lim AM, Chong SL, Ng YH, Chan YH, Lee JH, et al. (2020) Epidemiology and management of children with hypertensive crisis: A single-center experience. J Pediatr Intensive Care 9(1): 45-50.
- Falkner B, Daniels SR (2004) Summary of the fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Hypertension 44(4): 387-388.
- Grunwald JE, Pistilli M, Ying GS, Maguire M, Daniel E, et al. (2015) Retinopathy and the risk of cardiovascular disease in patients with chronic kidney disease (from the Chronic Renal Insufficiency Cohort Study). Am J Cardiol 116(10): 1527-1533.
- Sinha R, Raut S (2014) Pediatric lupus nephritis: Management update. World J Nephrol 3(2): 16-23.
- Szymanik GH, Kuźma ME, Małdyk J, Pańczyk TM (2016) Lupus nephritis in children - 10 years’ experience. Cent Eur J Immunol 41(3): 248-254.
Article Type
Case Report
Publication history
Received date: April 12, 2021
Published date: June 14, 2021
Address for correspondence
Nikhil Rajvanshi, Postgraduate, Department of Pediatrics, All India Institute of Medical Sciences, Rishikesh, India
Copyright
©2021 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Gokul RP, Nikhil R, Swathi C, Prashant kumar V. Lupus Nephritis: Viewing Kidneys Through Retinal Periscope. 2021- 3(3) OAJBS.ID.000293.
Figure 1: Fundoscopic image (A- right, B- left) with red free filter (c- right, D- left) showing multiple hemorrages (red
arrow), cotton wool spots (white arrow), perivascular clearing (blue arrow), hard exudates (black arrow) and optic
disc swelling (green arow), findings suggestive of malignant hypertension.
Figure 2: Optical coherence tomography showing bilateral cystoid macular edema- (A and C- Right eye; B and
D- Left eye): collection of fluid in intraretinal space, due to increased intravascular pressure and fluid exudationindicating
the possibility of central retinal vein occlusion.
Figure 3: Diethylenetriamine pentaacetic acid (DTPA) scan showing decreased contrast clearance from both
kidneys- plateauing of tracer levels in bilateral renal parenchyma and aorta- suggesting decreased Glomerular
Filtration Rate.
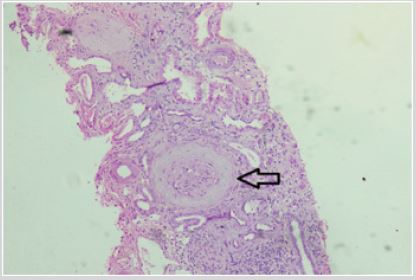
Figure 4: Photomicrograph (Hematoxylin and Eosin- 100X magnification) of renal biopsy specimen showing tubule
with squamous epithelium (red arrow) and intraluminal colloid deposition- suggestive of thyroidisation. Normal
glomerulus marked in black arrow.
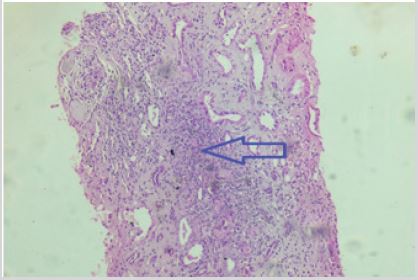
Figure 5: Photomicrograph of renal biopsy specimen (Hematoxylin and Eosin- 100X magnification) showing sclerosed
glomerulus with periglomerular fibrosis. Most of the glomeruli examined in other fields were also sclerosed, suggestive
of End Stage Renal Disease.
Figure 6: Photomicrograph of renal biopsy specimen (Hematoxylin and Eosin- 100X magnification) showing
inflammatory cells’ infiltration- predominantly lymphocytes with fibrosis in interstitium- suggestive of chronic
inflammation.