Is Obesity having a Role in Inducing Male Infertility?
ABSTRACT
Obesity is a worldwide problem among males and females of reproductive age. The increasing prevalence of obesity worldwide requires awareness of the negative impact of obesity not only on fertility but on human general health. This mini review aims to give a brief background about the current understanding of obesity and its role in inducing male infertility. A review was conducted using four electronic databases: PubMed, Web of Science, Google Scholar, and crossruff search for published studies on obesity and male infertility. The conclusion, obesity based on published data may have negative adverse on male fertility.
KEYWORDS
Obesity; Body mass index; Infertility; Spermatogenesis; DNA fragmentation
INTRODUCTION
Obesity and Infertility
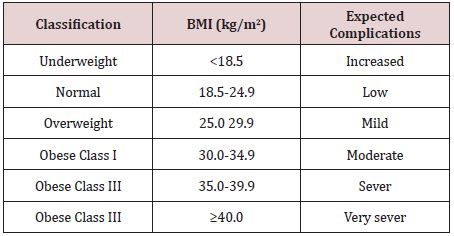
Obesity is defined as an excessive accumulation of fats in the body and causes serious medical conditions [1]. According to WHO “In 2016, 1.9 billion adults were overweight and 650 million were obese”. Obesity and overweight are classified by using a simple index called body mass index (BMI) [2]. The person is classified as overweight when the BMI is more than or equal to 25; and obese when BMI is over than or equal to 30, (Table 1) for BMI [3,4].
Hypotheses and Mechanisms of Obesity and Male Infertility
The mechanisms and hypothesis of obesity induced male infertility are still unclear. However, there are several causes of male infertility. Most of them are attributed to gonadal dysfunction or obstruction of the reproductive channels and chromosomal disorders [5]. Recently, there is another factor that may have participated with the previously mentioned etiologies in inducing male infertility [6]. This factor is obesity, affects male fertility either through hormonal imbalance or via the indirect comorbidities linked to diseases like arterial hypertension, diabetes, and high cholesterol levels. The previous studies have discussed several suggested hypotheses and mechanisms of male infertility that are related to obesity. The current article adopted the same previous ideas; the following paragraphs will discuss some of these mechanisms briefly.
Endocrinopathies
Endocrinal disturbances in obese males due to increased adipose tissues lead to sever alteration of spermatogenesis. The hormonal profile of obese males is characterized by elevated estrogen, leptin, and reduced sex hormone-binding globulin (SHBG). These hormones imbalance induce a negative feedback inhibition of the hypothalamus and pituitary gland, that may impact adversely on testosterone secretion due to deficiency of (GnRH)-luteinizing hormone (LH)/FSH ratio. As well as increased aromatization of peripheral testosterone into estrogen followed by inhibition of the hypothalmo- hypophyseal-gonadal axis (HPG) [7-9].
Sleep Apnea
A common sleep disorder that affects mainly obese patient is the obstructive sleep apnea, in which breathing pauses suddenly with irregular sleep rhythm during sleep, therefore, altered testosterone levels during night due to HPG axis dysfunction that caused by chronic hypoxia [10].
Insulin Resistance
Insulin resistance has been observed in obese male is relatively higher compared to normal BMI male. A high level of insulin in obese male leads to decreased hepatic production of sex hormones binding globulin (SHBG) [11]. SHBG is a blood transport protein for testosterone and estradiol, and affects directly or indirectly on androgen metabolism, and suggested to be one of the causative factors of infertility in obese male [12,13]. Secondary hypogonadism because of peripheral and central insulin resistance has been detected in obese men with type 2 diabetes [14].
Effects of Obesity on the Testicle Functions and Erectile Dysfunction
Increased level of estrogen in males is associated with obesity, which might effect on the spermatogenesis process [15]. Also, the impact of visceral adiposity and vascular endothelial activity might be the causative agent of erectile dysfunction in overweight men [16]. Lower circulating testosterone concentrations, cigarettes, intake of alcohol, diabetes, vascular diseases and psychological factors make a positive contribution to sexual dysfunction [17,18]. Furthermore, obese males might exacerbate psychogenic ED as corpulent individuals have such a lack of confidence, poor self- image, depression, anxiety, and poor self-esteem, thereby they consider themselves sexually repulsive or unwanted, thus attempting to avoid physical sexual intercourse [7].
Hyperthermia
Hyperthermia is defined as abnormal increasing in body temperature. In obese males, the excessive destruction of fat around suprapubic area causes hyperthermia that affects negatively on spermatogenesis and subsequently on other sperm parameters, however, this may be reversible in some infertile men [19].
Epigenetic Changes in Spermatogenesis
Epigenetic is a chromosomal modification of the gene’s expression and activity [20]. Sperm cells pass through extensive epigenetic modifications until becoming mature spermatozoon. These modifications are included but are not limited to DNA Methylation and histones [21]. The published data have shown hypomethylation has been associated with increased thresholds of sperm DNA damage and lower rates of pregnancy, while histones play a crucial role in preserving the DNA integrity of sperm [22,23]. Therefore, any abnormal alteration(s) in the above-mentioned processes could have a negative effect on sperm quality, pregnancy success, and offspring health. A recent study reported that the obese male has a high frequency of sperm epigenome [24].
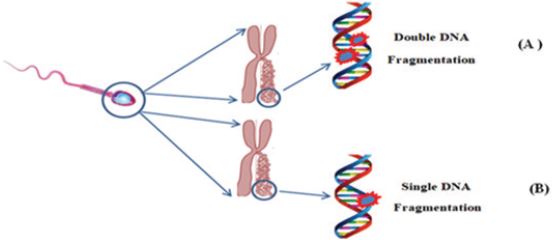
Normal Sperm DNA integrity is required for successful Assisted Reproductive Techniques (ART) and fertilization. This integrity is represented in normal movement and concentration of sperm, any defect in one of these factors may harm embryo development [25]. One study has reported that there may be a correlation between obesity and unsuccessful IVF process, whereas the rate of gestation loss was increased from 8.8% to 20% in obese males compare to males who have normal weight [26]. Male obesity is indicated as an underlying reason for both sperm count decline and infertility, as well as a rise in sperm DNA damage [27]. There are two types of DNA fragmentation; single-strand breaks (SSB) and double-strand breaks (DSB) are examples of DNA damage, (Figure 1) for DNA fragmentation examples.
In sperm DNA, both SSBs and DSBs can influence the overall libido and reproductive success. DSBs have been linked to recurrent miscarriages in couples without a female variable, also have a deleterious effect on embryo dynamics and implantation rates [28]. On the other hand, SSBs have no consequence on embryo growth or implantation rates, however, the greater levels of SSBs are associated with a negative gestation. Thus, SSB and DSB testing may be necessary for identifying the fertility of obese men’s sperm [29].
SUGGESTED MANAGEMENTS IN OBESITY ASSOCIATED MALE INFERTILITY
Changing Lifestyle
Reducing calorie intake, avoidance of junk fast foods, admission of antioxidants, and increasing energy consumption through exercises could contribute to minimizing the negative impacts of obesity on sperm quality and male fertility, as well as overall systematic health. There is agreement among some studies that people who lost weight via diet control and exercise reported a significant rise in levels of androgen and inhibin B and an enhancement in semen quality [30].
Pharmacotherapy
There are several pharmacological treatments, for instance, orlistat, topiramate/phentermine, lorcasen, bupropion/naltrexone, and liraglutide have been recommended to reduce weight and work through either appetite control or increased caloric burn [31]. Valuable insights into the pharmacological treatment of male infertility caused by obesity may include gonadotropin and/ or testosterone replacement therapy could use to reduce the quantity of leptin in circulation, but there is a lack of documented information to prove the efficacy of this medication [32].
Gastric Bypass (Bariatric Surgery)
For obese patients who failed to reduce their weight through exercises, diet, lifestyle management, and pharmacotherapy, surgical intervention is needed for example sleeve gastrectomy, gastric banding, and gastric bypass might be effective procedures, but studies on the usefulness of this particularity in improving semen parameters are still controversial [33-34].
CONCLUSION
Based on the previous studies, obesity may consider as one of the factors that play a significant role in induced male infertility. It may influence semen quality or trigger hormonal imbalance, such as lowering testosterone or elevating estradiol. Furthermore, it might affect negatively on Assisted Reproductive Techniques (ART) process and subsequently, lowering the pregnancy and live birth rates. However, reversing the adverse effects of obesity on male infertility could be possible either through treatment, exercise, or lifestyle management.
ACKNOWLEDGEMENT
Our great thanks to Dr. Alfatih Aboalbasher Yousif for his logistic support.
REFERENCES
- WHO (2021) Obesity and overweight.
- Haase CL, Eriksen KT (2020) Body mass index and risk of obesity-related conditions in a cohort of 2.9 million people: Evidence from a UK primary care database. Obesity science & practice 7(2): 137-147.
- CDC. About adult BMI - How is BMI interpreted for adults?
- Leisegang K, Sengupta P (2021) Obesity and male infertility: Mechanisms and management. Andrologia 53(1): e13617.
- Mamuna N, Kamal M (2017) Classification, causes, diagnosis and treatment of male infertility: a review. Oriental Pharmacy and Experimental Medicine 17: 89-109.
- Mammi C, Calanchini M, Antelmi A (2012) Androgens and adipose tissue in males: a complex and reciprocal interplay. Int J Endocrinol 2012:7 89653.
- Davidson LM, Millar K, Jones C (2015) Deleterious effects of obesity upon the hormonal and molecular mechanisms controlling spermatogenesis and male fertility. Hum Fertil 18(3): 184-193.
- Michalakisa K, Mintziorib G, Kaprarab A (2013) The complex interaction between obesity, metabolic syndrome and reproductive axis: A narrative review. Metabolism 62(4): 457-478.
- Karishma K, Ashok A, SS du Plessis (2012) A hormonal, physical and proteomic view of obesity-induced effects on male infertility and possible lifestyle modifications. Asian Pacific Journal of Reproduction 1(2): 161-168.
- Aydin B, Winters S (2016) Sex hormone-binding globulin in children and adolescents. Journal of Clinical Research in Pediatric Endocrinology 8(1): 1-12.
- Keevil BG, Adaway J (2019) Assessment of free testosterone concentration. J Steroid Biochem Mol Biol 190: 207-211.
- Molina VM, Muñoz GA (2018) Secondary male hypogonadism: A prevalent but overlooked comorbidity of obesity. Asian J Androl 20(6): 531-538.
- García-CE, Leibar A (2013) Risk factors and comorbidities and with erectile dysfunction. J Sex Med 10(10): 2529-2538.
- Erridge S, Moussa O, McIntyre C (2021) Obstructive sleep apnea in obese patients: A UK Population analysis. Obes Surg 31(5): 1986-1993.
- Ramy AG, Oleg S (2020) Peripubertal serum concentrations of organochlorine pesticides and semen parameters in Russian young men, Environment International 144: 106085.
- El Salam MA (2018) Obesity An enemy of male fertility: A mini review. Oman Med J 33(1): 3-6.
- Katsiki N, Athyros VG (2014) Reaching hypertriglyceridemia goals. Curr Med Res Opin 30(3): 391-393.
- Dandona P, Dhindsa S (2011) Update: Hypogonadotropic hypogonadism in type 2 diabetes and obesity. The Journal of Clinical Endocrinology and Metabolism 96(9): 2643-2651.
- Keevil BG, Adaway J (2019) Assessment of free testosterone concentration. J Steroid Biochem Mol Biol 190: 207-211.
- Oliveira PF, Sousa M (2017) Obesity, energy balance and spermatogenesis. Reproduction 153(6): R173-R185.
- Güneş S, Kulaç T (2013) The role of epigenetics in spermatogenesis. Turk J Urol 39(3): 181-187.
- El Hajj N, Zechner U (2011) Methylation status of imprinted genes and repetitive elements in sperm DNA from infertile males. Sex Dev 5(2): 60- 69.
- Nanassy, L, Carrell DT (2011) Analysis of the methylation pattern of six gene promoters in sperm of men with abnormal protamination. Asian journal of andrology 13(2): 342-346.
- Francis S, Yelumalai S, Jones C, Coward K (2014) Aberrant protamine content in sperm and consequential implications for infertility treatment. Hum Fertil (Camb) 17(2): 80-89.
- Houfflyn S, Matthys C (2017) Male Obesity: epigenetic origin and effects in sperm and offspring. Curr Mol Bio Rep 3(4): 288-296.
- Pearce KL, Hill A, Tremellen P (2019) Obesity related metabolic endotoxemia is associated with oxidative stress and impaired sperm DNA integrity. Basic Clin Androl 29(6).
- Provost MP, Acharya KS (2016) Pregnancy outcomes decline with increasing body mass index: analysis of 239,127 fresh autologous In vitro fertilization cycles from the 2008-2010 Society for assisted reproductive technology registry. Fertil Steril 105(3): 663-669.
- González MC, Gosálvez JR (2012) Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. International Journal of Molecular Sciences 13(11): 14026-14052.
- Chatterjee N, Walker GC (2017) Mechanisms of DNA damage, repair and mutagenesis. Environmental and Molecular Mutagenesis 58(5): 235-263.
- Sheena EM, Lewis (2013) The place of sperm DNA fragmentation testing in current day fertility management. Middle East Fertility Society Journal 18(2): 78-82.
- Patel D (2015) Pharmacotherapy for the management of obesity. Metabolism 64(11): 1376-1385.
- Rambhatla A, Mills NJ (2016) The Role of estrogen modulators in male hypogonadism and Infertility. Reviews in Urology 18(2): 66-72.
- Ronde DW, Jong FH (2011) Aromatase inhibitors in men: effects and therapeutic options. Reproductive Biology and Endocrinology 9: 93.
- Vincenzo DA, Busetto L (2018) Obesity, male reproductive function and bariatric Surgery. Frontiers in Endocrinology 18(9): 769.
- Claire C, Rachel L (2019) Changes in total sperm count after gastric bypass and sleeve gastrectomy: the BARIASPERM prospective study. Surgery for Obesity and Related Diseases 15(8): 1271-1279.
Article Type
Mini Review
Publication history
Received Date: March 14, 2022
Published: April 06, 2022
Address for correspondence
Nagia Suliman, Department of Clinical Chemistry, University of Gezira, Sudan
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Nafisa H, Maha M, Mayada K, Omer M, Nagia S, et.al. Is Obesity having a Role in Inducing Male Infertility?. 2022- 4(2) OAJBS.ID.000430.