Introducing Novel Flavour to Conventional Therapy Through AAC Evidence from Case Studies
ABSTRACT
Augmentative and Alternative mode of communication (AAC) is one of the emerging areas of intervention. The full potential of AAC especially as a support for already existing communication is still untapped. There are only very limited reports of case studies in AAC. In this paper we are presenting two cases in which AAC was used in alternative as well as augmentative form respectively. The cases have shown a good response towards AAC. The total communication in both the cases has improved with the use of AAC. Henceforth, we provide evidence to imbibe AAC during convention speech and language intervention for uplifting the total communication of the cases.
INTRODUCTION
AAC is an integrated group of components including symbols, aids, strategies, and techniques used by individuals to supplement any gestural, spoken and or written communication abilities ASHA 1991. Augmentative refers to the supplementation or addition to natural speech to enhance communication. Alternative refers to the substitution of another form of communication of natural speech Lloyd 1993; Becklman 1998 Typically AAC is described with respect to four components- symbol, aid, access technique and strategy. Symbol refers to the representation of target item in the AAC. It can be auditory, visual, tactile, kinesthetic or a combination of any of these.
The choice of symbol depends upon the client’s capacity. A matching must be made between the client’s abilities and his demands of communication which forms the basis for symbol selection. The next component in AAC is aid. This is applicable only in case of aided AAC and need not be considered for unaided AAC user. Aids can be low tech with minimal or no sophisticated technology involved (Ex.- communication book, communication board etc.) or high tech with sophisticated and/or dedicated software (Ex.-Tablets, Mobile phones etc.). Access technique refers to the means through which the user selects the symbol. It can be direct access by directly touching the symbol of indirect access by using external gadgets like wrist pointers, joysticks etc. strategy includes the process followed or adjustments made to ease into the use of AAC.
Examples of strategy can be reducing noise, maintaining eye contact with listener, carrying cue card with explanation of AAC etc. AAC is used by people who, some or all the time, cannot rely on their speech. AAC incorporates the individual’s full communication abilities and may include any existing speech or vocalizations, gestures, manual signs, and aided communication. AAC is truly multimodal, permitting individuals to use every mode possible to communicate. AAC is one of the widely accepted methods of communication intervention. AAC provides various channels to support or substitute communication for a patient. Recently, many studies have reported positive feedback regarding the effectiveness of imbibing AAC with traditional speech and language intervention. The support for AAC is garnered from the idea that providing yet another channel for communication in the form of augmentation or in severe cases alternative mode, can help in improving total communication of the patient, thereby helping in faster mainstreaming with minimum frustrations due to their lack of communication skills. Hence, recent years have seen a widespread increase in use of AAC. Over time, the use of AAC may change, although sometimes very slowly, and the AAC systems chosen today may not be the best systems tomorrow. AAC users encounter difficulty communicating via speech due to congenital and/or acquired disabilities occurring across the lifespan. These conditions include but are not limited to autism, cerebral palsy, dual sensory impairments, genetic syndromes, intellectual disability, multiple disabilities, hearing impairment, disease, stroke, and head injury.
AAC describes multiple ways to communicate that can supplement or compensate (either temporarily or permanently) for the impairment and disability patterns of individuals with severe expressive communication disorders. AAC for people with speech and language disorders is an interesting and challenging application field for research in Natural Language Processing. Strong language processing methods and adaptable linguistic knowledge bases are necessary for further advancements in the creation of AAC systems.
NEED FOR THE STUDY
It is highly essential to bring into light the value of inculcating AAC, especially in the case of severe motor speech disorders like cerebral palsy and childhood apraxia of speech. We present two cases wherein AAC was used as augmentative as well as alternative form of communication respectively.
AIM
To analyze Augmentative and Alternative communication as a futuristic approach to the management of children with motor speech disorders.
OBJECTIVES
Case 1
To implement AAC as an augmentative form of communication and train the child using AAC to improve the already existing communication skills.
Case 2
Implementing AAC as an alternative form of communication thereby providing a feasible channel for the child to communicate.
METHOD
Case 1
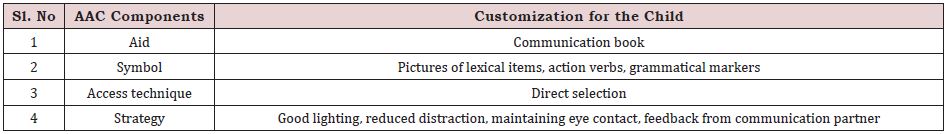
Speech and language intervention of a seven-year-old mild cerebral palsy child with spoken language disorder and sub average IQ was undertaken. The child did not have any sensory issues and showed only mild motoric weakness. He communicated functionally through single word utterances naturally augmented with personal gestures. We decided to provide AAC intervention in augmentative mode for children. Given below in Table 1 are the components of AAC chosen for the child.
The short-term goals implemented through AAC is as follows
a. To improve the identification and naming of common
lexical items
b. To increase the mean length of utterances
For attaining this goal, the interventionist used picture book as AAC. The interventionist would show the pictures of lexical items to the child and ask the child to name these pictures. If the child is unable to name them independently, the interventionist would provide multimodal cues. If the attempt yielded failure, the interventionist would name the target item and ask the child to imitate the name. Each item from the book was practiced thusly. The second goal was initiated after some items of the first goal were learnt by the child. For the second goal, the interventionist used the learnt names of lexical items and added grammatical markers like verb phrases, adverbs, conjunctions etc. and expanded the target from word level to sentence level (Figure 1).
Case 2
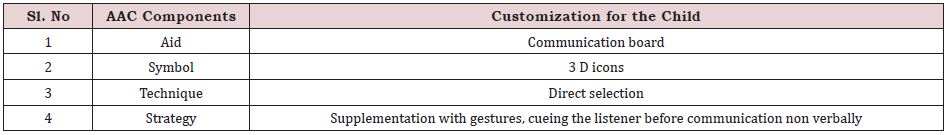
A seven-year-old child with severe cerebral palsy came to the department for speech and language intervention. The child was nonverbally barring some protowords, babbles and had not been attending proper intervention before coming to our department, because of which the child had very poor prelinguistic skills with no functional language abilities. Apart from this, the child was intellectually challenged and showed behavioral problems like tantrums, hyperactivity, and injurious behaviors. Due to all these reasons, AAC was introduced as an alternative form of communication (Table 2).
The goals planned for therapy were.
a. Establish reliable Yes / no system with sensory feedbacks
b. Improve functional communication
The AAC board was separated into two halves. First half consisted of three-dimensional icon for yes and no. Yes, was represented as a tick sign in green and no was represented as cross in red. Each of these symbols was mounted in a raised platform thereby giving a three-dimensional appearance. The other half of the board consisted of pictures of items used by the child in a dayto-day basis. Near each of these items a tactile stimulation patch was included (ex-velvet patch near plate, sandpaper patch near toilet etc.) to provide sensory feedback to the child whenever the child selects that item. Figure 2 shows the AAC board being used by case 2. AAC in Alternative mode used by case 2.
RESULTS
Case 1
AAC was very successful in the intervention of speech and language skills. The child could effectively use AAC for communicative purposes. His overall language skills improved in a significant manner.
On administration of Receptive expressive emergent language scale (Bzoch, League and Brown, 2006) after one month of AAC intervention, the child’s expressive skills drastically improved from 27 to 33 months (pretherapy) to 3-3.5 years. On administration of Linguistics Profile Test (Asha, 1997) the Child showed good phonemic discrimination, Phonetic expression, naming, and semantic discrimination. However, the language age remained below 6 years.
Case 2
Unfortunately, the case attended only a single session with AAC. The parents relocated and the child discontinued. However, during the sessions, the child was very co-operative and initiated the use of yes/no system for simple day to day questions like “do you like this?”, “do you want to play”? etc. Also, the child showed good response towards the sensory feedback in the functional communication half of sensory board.
However, time constraints prevented us from training using the board to improve functional communication. Consequently, the customized AAC was given to the mother and the interventionist demonstrated the training that must be done using the board. The parents were satisfied with the child’s response.
DISCUSSION
AAC is novel approach for the intervention of total communication in children. We decided to use AAC with traditional speech therapy in our cases due to a vast number of reasons. As far as case 1 was concerned, the child was older than six years and thus exceeded the sensitivity period for language stimulation. The child possessed good cognitive skills with a only a mild motor weakness. The child also showed good motivation with a supportive family. Also, the child comprehension was better thereby aiding in understanding of instructions. All of these reasons paved way to our decision to use AAC with traditional speech therapy. The use of AAC hastened the child’s prognosis. The child rapidly picked up new vocabulary and at the same time built his language usage by increasing the number of words per utterance. He also learnt to use proper grammatical markers along with strengthening the basic phonological awareness. From all of these results, we can effectively say that using AAC with traditional speech and language intervention would help in better and faster prognosis of the patient in case 2, the reasons for choosing AAC as alternative form of communication stemmed from child being more than 6 years old with severe intellectual disability and sensory- motor problems. Adding onto this is the fact the child has never attended a formal intervention before coming to our department leading to severe behavioral problems with negligible functional communication. However, due to the unavoidable reasons, the intervention did not follow a regular pattern. Nevertheless, the child showed good interest towards AAC in the session she attended. During the course of session, the child effectively started using yes/no system for communication with good attention towards the functional vocabulary on account of the sensory feedback provided near each symbol. This also supports the theory that AAC provides a good mode of communication especially in non-conventional cases. Similar results were obtained by [1] wherein the study suggested that intensive AAC, a multi-modal approach, and Rest improve speech accuracy and sentence length and complexity in children with moderate CP [2] also found evidence that AAC intervention has positive effects in decreasing challenging behavior for individuals with varying disabilities. Bob Williams, an expert communicator via augmentative and alternative communication (AAC), clearly articulates the singular importance of communication. Without access to effective communication, individuals with complex communication needs are consigned to live their lives with minimal means to express needs and wants, develop social relationships, and exchange information with others Blackstone 2007. The goal of intervention for individuals with complex communication needs is to support the development of communicative competence so that these individuals have access to the power of communication- to interact with others, to have an influence on their environment, and to participate fully in society Beukelman 2013. Communicative competence is essential to the quality of life of individuals with complex communication needs, for it provides the means to attain personal, educational, vocational, and social goals [3]. Alternative and augmentative communication technologies have the potential to increase the quality of care provided to patients with multiple disabilities; however, little work has been carried out in this area. Greater emphasis must be placed on affordable (high-tech) two-way communication aids that empower patients to become involved in decisions regarding their care. Quantitative evaluation methods should be used to discern the true benefits of such aids, and researchers should describe their study protocols in depth to promote replication and generalizability. The study findings point in the direction of more sophisticated futuristic approaches like Brain-computer interfaces (BCIs), which have the potential to improve communication for people who require but are unable to use traditional augmentative and alternative communication (AAC) devices. As BCIs move toward clinical practice, speech-language pathologists (SLPs) will need to consider their appropriateness for AAC intervention along with other futuristic approaches in the field of AAC [4,5].
CONCLUSION
AAC is a highly reliable & beneficial intervention strategy which helps in improving total communication. is AAC support communication, it does not limit it. Hence, practice of AAC should be implemented naturally during speech language intervention.
ETHICAL CONSIDERATION
The study followed the ethical rules and regulation of Kerala University of Health Sciences and was accepted by ethical committee of AWH Special College, Kozhikode. The client was informed, and consent was obtained. The study was conducted by maintaining proper respect and anonymity towards the client.
ACKNOWLEDGEMENT
We wish to thank our Principal Dr. P.K. Abdul Kader and our Head of the Department Mrs. Girija PC for allowing us to conduct this study. We also appreciate the support of staff and students of AWH Special College that helped us to achieve the completion of this study.
REFERENCES
- Korkalainen MJ, McCabe P, Smidt A, Morgan C (2022) Outcomes of a novel single case study incorporating rapid syllable transition treatment, AAC and blended intervention in children with cerebral palsy: a pilot study. Disability and Rehabilitation: Assistive Technology 16: 1-10.
- Walker V L, Snell ME (2013) Effects of augmentative and alternative communication on challenging behavior: A meta-analysis. Augmentative and Alternative Communication 29(2): 117-131.
- Light J, McNaughton D (2014) Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication? Augmentative and Alternative Communication 30(1): 1-18.
- Fossett B, Mirenda P (2007) Augmentative and alternative communication. In Samuel LO, Robert HH, Martha ES. (Eds.), Handbook on Developmental Disabilities. (Edn), The Guilford Press, USA, pp. 330- 348.
- Pitt KM, Brumberg JS, Pitt AR (2019) Considering augmentative and alternative communication research for brain-computer interface practice. Assistive Technology Outcomes and Benefits 13(1): 1-20.
Article Type
Research Article
Publication history
Received Date: September 30, 2022
Published: November 09, 2022
Address for correspondence
Nayana Narayanan, Department of Audiology and Speech Language Pathology, AWH Special College, India
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Nayana N, Labeeba K Akhila S, Fathima SKP. Introducing Novel Flavour to Conventional Therapy Through AAC Evidence from Case Studies. 2022- 4(6) OAJBS.ID.000514.