Incidental Finding of Bronchogenic Cyst During Laparoscopic Sleeve Gastrectomy
ABSTRACT
Background: Bronchogenic cysts are exceptional congenital malformations, mostly diagnosed in children, rarely in adults.
They are usually found in an intrathoracic region. We report a rare case of an intra-abdominal bronchogenic cyst located over the
gastroesophageal junction identified incidentally during a laparoscopic sleeve gastrectomy.
Case Presentation: A 37-year-old female with a BMI of 40 kg/m2 was admitted for a laparoscopic sleeve gastrectomy. During the
procedure, a bulging lesion was incidentally identified adherent to the gastroesophageal junction. An intra-operative gastroscopy
performed revealed signs of a mass effect above the GE junction and no signs of intra-gastric tumor. The decision of enucleation of
the cystic lesion and abortion of the sleeve gastrectomy was taken. Approximation of the esophageal muscular layer was performed
afterwards. The patient’s post-operative hospital course was uneventful and imaging results showed no leaks or abnormalities. The
final pathology results of the lesion revealed a bronchogenic cyst with no signs of malignancy.
Discussion and Conclusion: Management of an incidental tumor at the GE junction can be very challenging. In our case, we
opted for its resection while aborting the initial procedure to prevent further injuries to the esophagus. Excision of the tumor after
an EUS would have been a valid option as well. Therefore, we highly recommend routine gastroesophageal endoscopy prior to any
bariatric surgery.
KEYWORDS
Bronchogenic cyst; Enucleation; Laparoscopy; Sleeve gastrectomy
INTRODUCTION
Bronchogenic cysts are rare malformations of congenital origin derived from the abnormal budding of the primitive foregut [1,2]. They are usually located in the mediastinum or lung parenchyma and constitute the most common primary cysts of the mediastinum [2]. These lesions are mostly observed in infants and children, rarely in adults. They are more prevalent in males, with a 4:1 ratio [1]. Even though bronchogenic cysts are usually asymptomatic, it is important to note the risk of malignant transformation and increased risk of developing complications in adulthood, such as infection, hemorrhage, compression and pneumonia [2,3]. A definitive diagnosis is attained by histopathological examination. Imaging exams aid only in surgical planning; therefore, surgical resection is the recommended treatment in all suspected bronchogenic cysts. The most common approaches in adults are thoracotomy or thoracoscopy.
The prognosis of bronchogenic cysts is excellent after complete surgical excision [3]. Bronchogenic cysts located outside the thoracic cavity are very rare and are usually identified incidentally. They exhibit the same features as those found intrathoracically. Here we present a rare case of intra-abdominal bronchogenic cyst located over the gastroesophageal junction identified incidentally during a laparoscopic sleeve gastrectomy.
CASE PRESENTATION
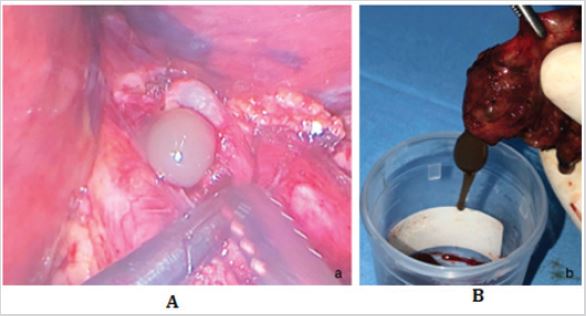
This is a case of a 37-year-old female patient with hypertension as her only past medical history who presented with a weight of 100kg and a height of 1.56 meters, resulting in a body mass index of 40 kg/ m2. This patient was morbidly obese and thus an excellent candidate for bariatric surgery. After discussing the options of her surgery, she decided on a laparoscopic sleeve gastrectomy. An informed consent was signed before she was taken to the operating room. The patient was put in a modified lithotomy position under general anesthesia; and after scrubbing and draping, pneumoperitoneum was established using a Veress needle. Upon entry to the abdomen, a 4cm x 5cm bulge adherent to the gastroesophageal junction was identified (Figure1a). Due to the fact that the lesion found was incidental and suspicious in nature and can therefore present a major threat to the patient’s life, the decision was taken to inform her family of her situation and obtain their consent for excising the mass. After being granted consent from her husband, we proceeded with the enucleation of the mass. Intra-operative gastroscopy was done in order to rule out intra-gastric tumor. The gastroscopy revealed normal gastric mucosa and no signs of a tumor; only a mass effect was noted, 2 to 3 cm above the GE junction. Enucleation of the mass was carried laparoscopically, during which the lesion appeared to be adherent to the muscular layer of the esophagus (Figure 1b). The cyst showed to be filled with vicious mucus (Figure 2a). The lesion was removed completely, and the cyst was nonseptate and containing around 20ml of vicious mucus brownish in color (Figure 2b). Approximation of the muscular layer using Vicryl 3.0 separate sutures was performed in an attempt to cope with the intraluminal pressure on the mucosa of the esophagus. The patient was kept NPO for the first 48 hours after surgery and an upper GI series with water-soluble contrast showed no leak and no delay in the passage of the contrast. The patient was started on a clear fluid diet for 7 days then progressed to a full liquid diet for another 7 days and then a soft diet for the next 7 days. After her discharge, the patient had a CT-scan chest -abdomen- superior pelvis, which revealed no other abnormal findings. Final pathology results of the lesion revealed a bronchogenic cyst with no signs of malignancies.
DISCUSSION
The majority of bronchogenic cysts are small and asymptomatic. Symptoms typically result from location rather than cyst size [4]. While subcarinal cysts may cause a persistent cough, bronchogenic cysts more distally in the tracheobronchial tree are frequently asymptomatic. Cysts along the esophagus or stomach may cause dysphagia due to their extrinsic compression [5].
Bronchogenic cysts arise during the fourth week of embryogenesis from the primitive foregut when a portion of the normal budding lung is pinched off and sequestered from the rest of the developing lung ending up most commonly at the subcarinal region [4,5]. Nevertheless, sub-diaphragmatic bronchogenic cysts can also be formed when cysts associated with the esophageal muscularis move distally along with the rapidly migrating esophagus after the development and septation of the trachea-esophageal groove and before the fusion of the diaphragmatic components. When these cysts sequester early enough, they can separate completely from the developing foregut structures and thus form the reported supradiaphragmatic and sub-diaphragmatic bronchogenic cysts that can be located in the diaphragmatic muscle, the small bowel mesentery, the pericardium, the retroperitoneum, and the pre-sternal skin [5].
A bronchogenic cyst outside the thoracic cavity is very rare and in most cases is found incidentally in the course of a computer tomography (CT) as a retroperitoneal mass, but a pure intraabdominal location is extremely uncommon [6]. Sub-diaphragmatic bronchogenic cysts present a diagnostic challenge. The differential diagnoses include gastrointestinal stromal tumors, leiomyomata, pancreatic cystic neoplasms, and esophageal duplication cysts in addition to sarcoma [5]. On a CT scan, bronchogenic cysts appear as a well-defined cystic lesion with or without calcifications. On a magnetic resonance imaging (MRI), the lesion appears as isointense to hyper-intense on T1-weighted images and hyper-intense on T2-weighted images resembling solid tumors like GIST with cystic degeneration [4]. Endoscopic ultrasound (EUS) may help in determining the exact location of the cyst within the gastric wall, while a CT scan or EUS guided needle biopsy may reveal mucoid material providing a clue towards the correct diagnosis [4].
The surgical procedure of choice for bronchogenic cysts is enucleation of the cyst with its entire lining en bloc [7]. As malignancy is rare, wide margins of resection are not necessary and often not possible [7,8]. Subdiaphragmatic cysts are typically approached through a laparotomy or laparoscopy [8]. Preoperative biopsy of the cyst through EUS-guided techniques is not contraindicated even for periesophageal cysts despite the older, now-defunct notion that preoperative biopsy of submucosal esophageal lesions leads to increased intraoperative mucosal injury [9]. In addition to thoracoscopy, newer minimally invasive techniques have been developed to treat bronchogenic cysts. Cyst drainage through endobronchial ultrasound or esophageal ultrasound guidance has been described [9]. Despite the high risk of cyst recurrence and the need for multiple procedures, this has become an attractive option, particularly in the management of frail patients or in the acute phase of cyst infection [7.8]. Although data supporting these minimally invasive approaches are sparse, and the true rate of symptomatic cyst recurrence is lacking, endoscopic drainage has gained popularity in recent years [5]. Bronchogenic cysts are most commonly asymptomatic and are usually found incidentally which raise doubts about the most appropriate management of this disease. The current trend to surgical excise those tumors is mainly due to possible complications from these masses, such as infection, bleeding, malignant transformation and the lack of a certain pathological diagnosis [6].
Bronchogenic cysts are lined with a single layer of ciliated columnar mucosa that may be pseudostratified. The remaining thin wall of the cyst is comprised of fibrous tissue and mucin-secreting cells. The cyst cavity is most commonly non-septated and filled with a sterile fluid comprised of mucous and sloughed respiratory epithelial debris [5].
In our case, we incidentally identified a sub-diaphragmatic mass over the GE junction during a laparoscopic sleeve gastrectomy. Intraoperatively, we were able to carry the operation laparoscopically and we opted for an enucleation as described in previous literatures [7]. Laparoscopy is considered a safe method when managing such a tumor, and if dealt with expert hands, low risk is faced concerning injury to the esophagus, or dissemination in case of other pathology [7,8]. Surgery is always recommended to prevent serious complications in symptomatic and asymptomatic cases [9,10]. An additional option to reduce concern would have been if a Dor fundoplication was performed post enucleation of the tumor in order to manage any possible micro injury to the esophagus or a future GERD that can arise due to change in intraesophageal pressure [7]. We opted to abort the initial sleeve gastrectomy after the enucleation of the lesion in order to wait for the final pathology result of the tumor and to reduce the high gastric pressure that can be caused after the sleeve gastrectomy. Finally, due to the mass effect created by the tumor over the GE junction in addition to other possible eso-gastric pathologies that can be identified in the pre-operative phase, we recommend routine gastroesophageal endoscopy prior to any bariatric surgery.
CONCLUSION
As a conclusion, an incidental finding of bronchogenic cyst outside the thoracic cavity is very rare. Here, we report the finding of a bronchogenic cyst at the GE junction during sleeve gastrectomy. We opted for its resection and aborted the initial procedure due to the high pressure on the esophagus that can result from the sleeve gastrectomy, thus putting the patient at risk. In retrospect, abortion of the whole procedure without excision of the tumor prior to an EUS could have also been a valid option due to risk of sarcoma. Therefore, routine gastroesophageal endoscopy is highly recommended prior to any bariatric surgery. Finally, management of an incidental tumor at the GE junction can be very challenging due to various pathologies that can be faced; the absence of consensus to whether the initial procedure can be carried on or aborted should be more elaborated and studied in the future.
REFERENCES
- Santos I, Barros J, Lopes T, Mesquita M, Barroso L, et al. (2019) Bronchogenic cyst of the neck in an elder patient: A case report. International Journal of Surgery Case Reports 64: 128-132.
- Aktoğu S, Yuncu G, Halilçolar H, Ermete S, Buduneli T, et al. (1996) Bronchogenic cysts: clinicopathological presentation and treatment. The European Respiratory Journal 9(10): 2017-2021.
- Limaiem F, Mlika M (2020). Bronchogenic Cyst. In Stat Pearls. Stat Pearls Publishing, USA.
- Chhaidar A, Ammar H, Abdessayed N, Azzaza M, Gupta R, et al. (2017) Large bronchogenic cyst of stomach: A case report. International Journal of Surgery Case Reports 34: 126-129.
- Ballehaninna U K, Shaw J P, Brichkov I (2013) Subdiaphragmatic bronchogenic cyst at the gastroesophageal junction presenting with Dysphagia: A case report. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 23(4): e170-e172.
- Díaz N, Naranjo T, Gómez A, Ruiz RF, Pérez M, et al. (2010) Intraabdominal bronchogenic cyst. Journal of gastrointestinal surgery: official Journal of the Society for Surgery of the Alimentary Tract 14(4): 756-758.
- Tonouchi A, Kinoshita T, Sunagawa H, Hamakawa T, Kaito A, et al. (2016) Bronchogenic cyst at esophagogastric junction treated by laparoscopic full-thickness resection and hand-sewn closure: A case report. Surgical Case Reports 2(1): 41.
- Zügel NP, Kox M, Lang RA, Hüttl TP (2008) Laparoscopic resection of an intradiaphragmatic bronchogenic cyst. JSLS: Journal of the Society of Laparoendoscopic Surgeons 12(3): 318-320.
- Chen T J, Liao C H, Shen T C (2018) Bronchogenic cyst. QJM 111(12): 905.
Article Type
Case Report
Publication history
Received date: February 15, 2021
Published date: July 08, 2021
Address for correspondence
Raja Wakim, Head of General Surgery Department - Mount Lebanon Hospital University Medical Center, Lebanon
Copyright
©2021 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Toufic S, Omar T, Murielle ElF, Elissa M, Raja W. Incidental Finding of Bronchogenic Cyst During Laparoscopic Sleeve Gastrectomy. 2021- 3(4) OAJBS.ID.000301.
Figure 1: A- Mass over the gastroesophageal junction causing mass effect. B- Enuclation of the mass done after
identification of a cleavage plane.
Figure 2: A- Cyst showing viscous mucus contents intra-abdominal. B- Removal of the cyst with a size 5cm x 4cm
containing viscous mucus and sticky content with absence of septation in the cyst.