Comfort Care Decision in an Infant with Medical Complexity
ABSTRACT
Children with medical complexity account for approximately 10% of pediatric admissions. Many of the problems of the infants with medical complexity are noticed or projected in the neonatal period. The role of neonatal intensive care unit (NICU) staff is therefore very important in these cases. Infant with medically complexity and those who are technology-dependent may benefit from an early comfort care discussion. We present a case of such an infant in whom a comfort care decision was made in the NICU resulted in a peaceful death, saving the infant from many invasive life-sustaining procedures and interventions.
ABBREVIATIONS:
NICU: Neonatal Intensive Care Unit
INTRODUCTION
Children with medical complexity account for approximately 10% of pediatric admissions. Advances in the intensive care practices, technological devices, and improved survival continue to increase both the numbers and complexity of these children cared for both in the hospital and at home. In addition to the time, the impact of social, financial, and emotional burden on the parents are often under looked. Many of the problems of the infants with medical complexity are noticed or projected in the neonatal period. The role of neonatal intensive care unit (NICU) staff is therefore very important in these cases. Infant with medically complexity and those who are technology-dependent may benefit from an early comfort care discussion. An informed parent who understand the ramifications of the long term follow up and outcome could be talked into the concept of what is in the ‘best interest’ of the infant earlier rather than later.
In addition to ethical principles, many factors contribute to the comfort care decision, viz. religious inclination, societal pressures, parental guilt, etc. In this paper, we present a case of infant with medical complexity, in whom a comfort care decision was made in NICU that resulted in a peaceful death, saving the infant from many invasive life-sustaining procedures in the NICU and later unwarranted hospital admissions and interventions. Currently we don’t have any pediatric palliative team at our hospital to provide a detail consultation that involves relief from pain and other symptoms while focusing on the infant as a whole, taking into consideration physical, emotional, spiritual, and social needs, along with the needs of the family members.
CASE PRESENTATION
A premature boy is delivered at 25 3/7 weeks to a 19-year-old G2P1001 mother. She presented to labor and delivery secondary to abdominal pain and vaginal bleeding. All prenatal labs were including RPR, HIV, hepatitis B, chlamydia and gonorrhea were negative.
Rupture of membrane was at delivery with clear fluids. At delivery, infant had no cry, no respiratory effort, and no tone. He was resuscitated and then transported immediately to the neonatal intensive care unit (NICU). Apgar scores were 1/4/6, at 1/5/10 minutes. Cord blood gas showed a pH of 7.13, PCO2 of 42, PO2 of 37 and HCO3 of 12.7. Infant had a very stormy course.
CLINICAL COURSE
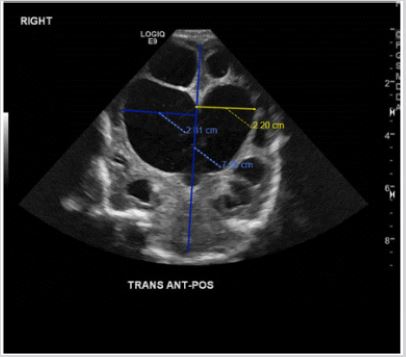
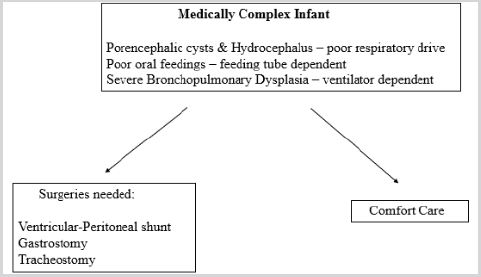
During his 3-month stay in the NICU, he developed respiratory distress syndrome with pulmonary insufficiency, pneumothorax, patent ductus arteriosus, grade 4 intraventricular hemorrhage, grade 4 periventricular leukomalacia (Figure 1), seizures and poor oral feeding. The infant was unable to wean from the noninvasive ventilator support. The NICU staff has divided views on the management of this technology dependent infant (Figure 2). Some wanted full code status for the infant, including tracheostomy gastrostomy, ventricular shunt, and home ventilator. While others were in favor of no escalation in medical therapy. In view of the infant’s dependent state, poor neurodevelopmental outcome and need for continuous medical support, a decision of comfort care was made. However, infant continued to have reservoir tap periodically. The team of consultants decided not to perform the brain perfusion scan or any other neurological procedures. As infant has multiorgan diseases, he was not a candidate for organ donation, we did not perform apnea test or brain death studies. The infant has agonal breathing pattern most likely due to extensive brain damage.
After multiple discussion with the family, it was decided to do not attempt resuscitation and forgoing any invasive procedure. On our first meeting and discussion about comfort care, parents were upset, especially the mother. In the second sitting, father looked more comfortable with the palliative care plan and mother still wanted more time. Five days into the decision, parents noticed the infant’s agony, they finally agreed to the comfort care. Respiratory support was removed, and infant was fed by a nasogastric tube. Oral morphine was provided for pain. Religious ceremony was done in the NICU. Infant was roomed in with parents. The same night, the infant died peacefully in parents’ arms.
DISCUSSION
In the resource rich institutions, doing everything is not only possible but viewed as mandatory. However, is it wise to do so? Every investigation and procedure have a cost. It might not come from the private insurance company or parents’ pockets, but it is a burden to state and federal health budget. Keeping religion, ethical and social aspect aside, what medical benefits are gained by intensive management of technology dependent neurologically affected infants? Would they become a contributor to the society, or they would be another consumer? Let us look at the case and try to answer these questions. The sweet boy described above had no functioning brain left due to the course of his neurological damage caused by severe intraventricular hemorrhage and periventricular leukomalacia.
He cannot be fed orally, and he cannot breathe without respiratory support. In view of his loss of brain tissue, the chances of improvement in his neurological status was zero percent. We could have the surgery team perform tracheostomy, gastrostomy and ventricular shunt but would these procedures have changed his life? The scientific answer is no. By performing life sustaining procedures, the infant would be added to the medically complex children pool. Would that be right for him and his family?
Comfort care decisions are not easy. We recently elucidated on this by describing a case of a newborn infant that had severe microcephaly and imperforate anus. There is a critical knowledge gap in understanding the role of comfort care in medically complex cases [1]. In cases with known genetic diseases and chromosomal anomalies, the decision of comfort care is often difficult [2-4]. Also delineating end stage brain diseases with severe technologically dependent status is difficult. However, the NICU team agreed on the therapeutic futility.
The survival statistics also varies in certain cases, however, in newborn with end stage brain diseases or severe technologically dependent status, comfort care plan should be offered to the families, as presented in the article. We need many more case presentations like this one and should have regular conferences to incorporate parental views to better understand the complexity of technological dependent infants and their sufferings. It is not about what we could do, but it should be about we should do.
ACKNOWLEDGMENT
I would like to thank the parents, social worker, and staff nurses for their complete support to the decision of comfort care.
REFERENCES
- Manzar S (2019) Uncomfortable comfort care. Acad Pediatr 19(8): 853- 854.
- Diekema DS, Botkin JR (2009) Committee on bioethics clinical reportforgoing medically provided nutrition and hydration in children. Pediatrics 124(2): 813-822.
- Carter BS, Leuthner SR (2003) The ethics of withholding/withdrawing nutrition in the newborn. Semin Perinatol 27(6): 480-487.
- Bidegain M, Younge N (2015) Comfort care vs palliative care: Is there a difference in neonates? Neo-reviews 16: e333-e339.
Article Type
Case Report
Publication history
Received date: July 07, 2020
Published date: July 23, 2020
Address for correspondence
Shabih Manzar, MD, Department of Pediatrics, College of Medicine, Louisiana State University of Health Sciences, USA
Copyright
©2020 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Manzar S. Comfort Care Decision in an Infant with Medical Complexity. 2020 - 2(4) OAJBS.ID.000196.
Figure 1: Head ultrasound (coronal image) at 3 months of age showing marked hydrocephalus and porencephalic changes bilaterally with marked thinning of the abnormal cerebral cortex. The right lateral ventricle index measures 2.8 cm with the left measuring 2.2 cm.
Figure 2: Schematic representation of options in the case presented.