Assessment of Medication Errors in Emergency Ward at Nekemte Referral Hospital, West Ethiopia
ABSTRACT
Background: Medication error is defined as failure in the treatment process that leads to or has the potential to lead to harm
to the patient. It may occur at each five stages of drug ordering and delivery including prescription, transcription, dispensing, and
administration or monitoring. Prevalence of medication error in healthcare settings have been found that they were common in
hospitals. A significant proportion of medication errors are associated with actual or potentially harmful effects.
Objective: The major goal of this assessment was to figure out the actual practices on the ground in medications administered
in NRH emergency ward, emphasizing on distribution and prevalence of errors.
Methods: This study was a cross-sectional retrospective study conducted at medical and pediatrics wards of NRH.
Results: To meet objectives, 768 prescription papers were used to collect necessary data within this study period. A total of
768 patient’s medical prescription orders, there were about 71.73% of at least one prescription error when it is compared to
standard prescription order. Of this medication error prevalence, the number of prescriptions with low dose (35.93%) number
of prescriptions without appropriate indication (26.43%) number of prescriptions with too high-dose (3.13%) number of
prescriptions with inappropriate interval (2.73%) number of prescriptions with drug interaction (1.95%) number of prescriptions
with contraindication (1.56%). Numbers of prescriptions with 1st line medicine indicated for diseases were 1.43%. Of total sampled
prescriptions, the numbers of drugs order per the number of prescriptions were two. There were prescriptions without patient
address (99.35%), prescriptions without card number (97.40%) prescriptions without date (60.94%) prescriptions without sex of
patients, (13.02%) prescriptions without age of patients (8.85%).
Conclusion and Recommendation: There were clear and large medication and prescription errors on medication prescribing
and administration practices in NRH emergency ward. Every member of clinical team had better strive to perform sound performance
standard to ensure maximum patient therapeutic outcome as long as negligence and carelessness must not make a patient life to
be claimed.
KEYWORDS
Medication error; Pharmaceutical care; Emergency ward; Nekemte Referral Hospital
INTRODUCTION
Medication errors (MEs) are issues in health care and are probably one of the most common types of medical errors [1]. MEs have been defined as “failure in the treatment process that leads to or has the potential to lead to harm to the patient”. It may occur at each five stages of drug ordering and delivery including prescription, transcription, dispensing, and administration or monitoring [2]. Prescribing and drug administration appear to be associated with the greatest number of MEs, whether harm is caused or not. Recent systematic reviews of medication administration error (MAE) prevalence in healthcare settings found that they were common, with one reporting an estimated median of 19.1% of ‘total opportunities for error’ in hospitals. A significant proportion of MAEs are associated with actual or potentially harmful effects [3]. Prescription of drugs can be divided into an intellectual partdecision making, i.e. knowledge of diagnosis, interactions, and contraindications, and a technical part including communication of essential information, i.e. drug name, dose form of administration [4]. Medicine is usually prescribed by the doctor and dispensed by the pharmacist, but responsibility for correct administration that could be responsibility of the nurse includes preparing, checking and administering medications, updating their knowledge about medications, monitoring the effectiveness of treatment, reporting adverse reactions and teaching patient about their drugs. So, errors include wrong as well as missing actions [5].
MEs contribute to the morbidity and mortality of hospitalized patients [6] and can result in hospitalization or death of a patient [7]. In addition, MEs can affect patients, families, and health care providers indirectly because of cost implications, and psychological impact, since errors erode public confidence in the health care service [1]. In the USA, MEs have been found to be responsible for 7,000 patient injuries per year, with a similar incidence and consequences in the UK. Approximately one third of adverse drug events (ADEs) is associated with medication errors and is thus preventable. MEs occur in 6.5 of 100 adult medication orders [6].
Emergency departments (EDs) are characterized by simultaneous care of multiple patients with various complex medical conditions most of them are acutely ill. Large volume of patients with complex diseases seeking medical treatments, medical information gaps among them, speed and complexity of medication use, working in under-staffing crowded environment and in hard conditions such as disrupted sleep cycles, multiple interruption, acute time constraint and prevalent verbal ordering are contributing causes for medication errors by emergency care providers [5].
Lack of point of care reference information, alertness of the health professional, and patient information gap are also known for their role in medication error [8]. It has been claimed that drug therapy is the common intervention prescribed by physicians, and the distribution and administration of medication represents a major duty of hospital-based pharmacists and nurse. A survey report from the United States (2007) showed that 97% of nurses in the country were worried about medication errors. And nearly all (99%) believe that there is a grave risk to patients if errors occurred [9]. MEs occur in 2-14% of hospitalized patients and lead to 44,000-98,000 annual deaths in the United States. Medication errors rates have been estimated between 4% and 14% in EDs and even higher among pediatric EDs [2]. However, data regarding MEs in Africa especially in Ethiopia is scarce at least in this study area.
METHODS
Study Setting
Nekemte Town is located in the western part of Ethiopia. The study was conducted at Nekemte Referral Hospital (NRH), in Nekemte Town, which is about 331km west of Addis Ababa. It is one of main referral hospitals in western regions of Ethiopia. NRH has eleven [10] main wards. Of these, emergence ward is one, and have eleven [11] beds.
Study Design
A retrospective, quantitative, and cross-sectional survey designed to describe the current medication practices at Nekemte Referral Hospital, emergency ward was used. About 768 prescription papers were systematically selected after being arranged by prescription date wise arrangement. Then, information related to the study objectives were collected from each [12-18].
Data Collection and Analysis
One trained pharmacy personnel collected data on check list by observing collected patients’ prescriptions and medication records. The specific types of data necessary to measure medication errors were recorded for each prescription and entered directly into prepared medication error check list form. All data were first analysed manually and then using Microsoft Excel 2007. In the statistical analysis, frequencies, averages/means, standard deviations and percentages were obtained.
Ethical Consideration
Ethical approval was obtained from the Wollega University Research Vice President and Nekemte Referral Hospital. Then, written informed consents were collected from patients or care givers before data collections [18-25].
RESULTS AND DISCUSSION
Samples of 768 prescriptions were identified and assessed in the emergency ward of Nekemte Referral Hospital. Data was collected and analysed on the line of its objectives and presented below:
Demographic Details and Characteristics of Patients
A total of 768 patient’s medical prescriptions were observed and patient’s information’s were reviewed during data collection period. From these, 54.69% were female and 45.31% were male patient’s prescriptions. There were about 1,536 drugs orders on 768 prescription papers. So, the prescription orders per the number of prescriptions were 2.0 (1536/768). This average (2.0) is higher compared with the standard (1.6-1.8) derived as ideal [26]. In a similar study performed in southwest Ethiopia at Jimma Hospital, the average number of drugs per encounter was 1.59, which was in the acceptable range [23].
However, in a study on prescribing patterns in three hospitals in north Ethiopia, the average number of drugs per patient was 0.98 at Gondar Hospital, 1.8 in Bahirdar Hospital, and 2.2 in Debre Tabor Hospital [24]. A national baseline study on drug use indicators in Ethiopia in September 2002 also found the average number of drugs prescribed per encounter to be 1.9, which is similar to this finding [25]. Reasons of high average number of drugs per encounter might be due to shortage of therapeutically correct drugs; and/or lack of prescribers’ therapeutic training; and/or lack of appropriate diagnostic equipment’s; and/or un reliable prescribers ability to diagnose and treat common illness or may be prescribers were influenced by patients demands [27]. Concerning patient’s related information, the most existing medication errors in the emergency department as shown below (Table 1).
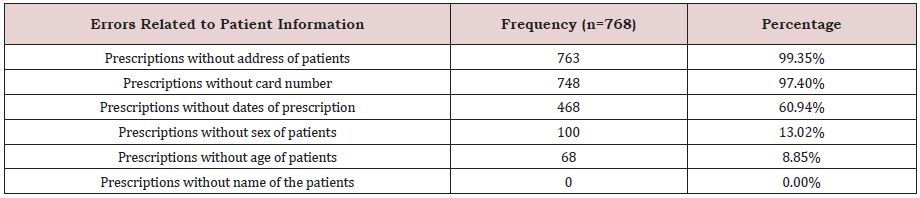
Of these errors related to address of patient bearing prescription holds the largest (99.35%) followed by card number bearing quantity error (97.40%) and error related to date of prescription (60.94%). The study has also revealed that 13.02% of prescriptions had not sex of patients, while 8.85%of prescriptions hadn’t shown the age of patients for which medications were ordered. On the other hand, there was no error related with writing of the name of patient on the prescriptions.
According to study done in Iran, the most medication errors occurred at administration of patient’s information (36%) with the most common type of improper writing of the patients age (18% of errors) followed by sex and date of the admission with the rate of 11% [2]. Furthermore, the study done at ICU in Jimma University specialized Hospital medication administration interventions, more than half (51.8%) were labelled as medication errors related with patients information such as omission of patient age, sex and card numbers of 30.3%, 29, 18.3% of the medication administration errors, respectively [9].
Medication Error Related to Prescriptions
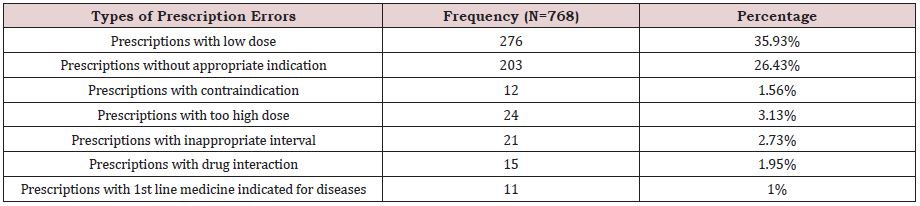
Of total of 768 patients’ medical prescription orders, prescriptions with low dose hold major encountered errors (35.93%), followed by inappropriate indications (26.43%). In addition, there were significant errors such as prescription with too high dose (3.13%) and prescriptions with inappropriate interval (2.73%) (Table 2). Thus, this has shown that 71.73% of prescriptions were with different types of errors in emergency department. It is also important to mention that only 1.43% of medications of first line have been ordered for patients in the ward. Also, there were drugs which were ordered even though there were contraindication (1.56%) and drug interaction (1.95%). Inappropriate use and overuse of medicines waste resources - often out-of-pocket payments by patients and result in significant patient harm in terms of poor patient outcomes and adverse drug reactions.
The Top Ten Prescribed Antibiotics In NRH
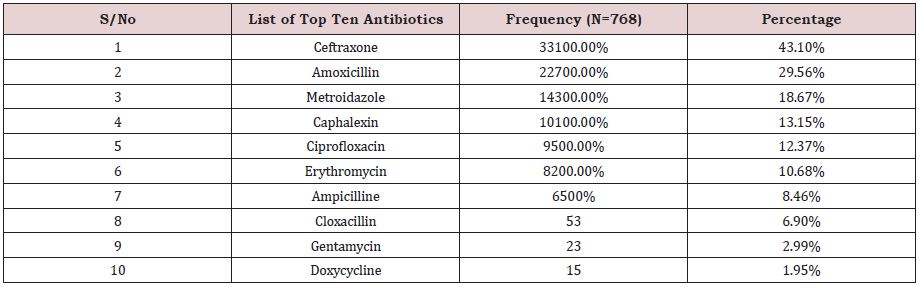
In this study, the top ten prescribed antibiotics drugs were examined along with the study of patient’s information and prescriptions orders in emergency department. The top ten antibiotics drugs in NRH emergency ward were summarized under (Table 3) below. Accordingly, the frequency of ceftriaxone (43.10%) was highest. Amoxicillin stands at the second (29.56%), followed by metronidazole (18.67%). On the other hand, doxycycline accounted the least frequency (1.95%).
Error Related with Adequacy of Drug Storage and Dispensary
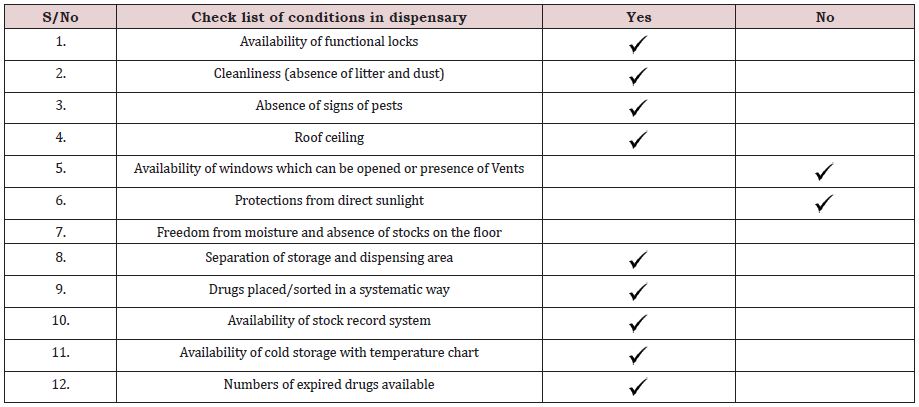
Many studies show that the quality of drug is important to enhance public health in developing countries. Hence, to this effect the purpose of this indicator is to determine the status of essential drugs storage in public health care facilities and regional drug stores as one factor that affects drug quality. This study addressed errors related with adequacy of drug storage and dispensary in light of eleven conditions provided below. According to different studies, appropriate drug storage system has direct effect up on the quality of the drugs. To this end, the condition of NRH drug store has examined by the checklist provided below in (Table 4). According to the result NHR has functional locks, roof ceiling, and separated store from dispensary, systematic way of drug placement, stock record system, and cold storage with temperature chart. Moreover, there was no sign of pests and expired drugs. However, the sore has problems with cleanliness (absence of litter and dust) in some parts. It has no sufficient windows which can be opened or presence of vents. The system of drug protection from direct light is not sufficient. In addition to this, there was no sufficient freedom from moisture and stock on the floor.
According to many scholars’ studies, appropriate dispensary system has direct effect up on the quality of the drugs. To this end the condition of NRH drug store has examined by the checklist provided below in (Table 5). Accordingly, NHR has functional locks, roof ceiling, cleanliness and separated store from dispensary, systematic way of drug placement, stock record system, and cold storage with temperature chart. Moreover, there was no sign of pests and expired drugs. However, there were no sufficient windows which can be opened or presence of vents. The system of drug protection from direct light is not sufficient. In addition to this, there was no sufficient freedom from moisture and stock on the floor. This indicates that the sore and dispensary sections were with some problems and factors that affect drug qualities.
CONCLUSION
Based on the findings of this study, the medication errors were high at the study area. There was high prevalence of medication error at NRH, emergency ward. The most prevalent types of medication errors occurred were prescriptions with low dose, inappropriate indications, too high dose, prescriptions with inappropriate interval and lack of full patient information.
RECOMMENDATION
Authors recommend all concerned body to incorporate clinical pharmacist in pharmaceutical care decision making; act according to national standard treatment guidelines; establishing drug and therapeutic committee; problem-based basic training in pharmacotherapy; drug information centres establishment; expansion of drug use evaluation system and preparation and dissemination of drug bulletins.
ACKNOWLEDGEMENT
We thank Wollega University Research Vice President Office and Nekemte Referral Hospital for allowing and helping us to conduct this research. Also, we extend our gratitude to NRH staffs for their good cooperation’s.
REFERENCES
- Asrat A, Yamane A, Worku B, Mrkuzie W (2011) Medication prescription errors in ICU of JUSH. International Archives of Medicine April.
- Alireza Z, Mohammad T, Amir N, Simin D (2013) Frequency and types of the medication errors in an academic emergency department in Iran: the emergent need for clinical pharmacy services in emergency departments. journal of Research in Pharmacy practice 2(3):118-22.
- Richard N, Steven D, Jonathan C, Darren M (2013) causes of Medication Administration Errors in Hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf 36(11): 1045-1067.
- Mohammad A (2011) Factors contributing to medication errors in Jordan: Iran J Nurs Midwifery Res Spring 16(2):158-61.
- (1993) ASHP guidelines on preventing medication errors in hospitals. Am J Hosp pharm 50(2): 305-14.
- Rebecca H, Patricia AH (2013) A study on information induced medication errors. Australian Health informatics and security conference.
- Jenkins G, Johnston PE, Patel NR, Jones I, Aronsky D (2006) The epidemiology of medication prescribing errors in the emergency department. AMIA Annu symp proc 968.
- Asrat A, Yamane A, Worku B, Mrkuzie W (2012) medication administrator errors in an intensive care unit Ethiopia. Archives of pharmacy practice 5(1):15.
- Nahid K, Mani M, Hussein S, Marzieh H, Mahdi R (2012) What are patients’ concerns about medical errors in an emergency department? Itan Qaboos Univ Med J 12(1):86-92.
- Medication Errors (2011).
- Bates DW, Boyle DL, Vander VMB, Schneider J, Leape L (1995) Relationship between medication errors and adverse drug events. J Gen Intern Med 10(4):199-205.
- Kaushal R, Bates DW, Landrigan C, Mckenna Kj, Clapp MD, et al. (2001) Medication errors and adverse drug events in pediatric inpatients. J Am Med Assoc 285: 2114-2120.
- CA Bond, Cynthia LR, Todd F (2001) Medication errors in United States hospitals. Pharmacotherapy 21(9): 1023-36.
- Jennane N, Madani N, Rachida O, Abide K, Khoudri I, et al. (2011) Incidence of medication errors in Moroccan medical intensive care unit. Int Arch Med 4: 32.
- Feleke Y, Girma B (2010) Medication Administration errors involving pediatric in-patients in a hospital in Ethiopia. Trop J pharm Res 9(4): 401-407.
- Gideon N, Yonatan K, Segewkal H (2013) Medication errors in the adult emergency unit of a tertary care teaching hospital in Addis Ababa. Arch Pharma pract 4(4).
- David C, Melanie R, Lauren E, Sarah J (2012) Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems. Agency for Healthcare Research and Quality 12(1): 86-89.
- Philip S, Marc A, Tanya C, Xiaoqing X, Antoinette C, et al. (2014) Detection and correction of prescription error by an emergency department. CJEM 16(3): 193-206.
- Naoual J, Naoufel M, Rachida O, Khalid A, Ibtissam K, et al. (2011) Incidence of medication errors in a Moroccan medical intensive care unit. International Archives of Medicine 4: 32.
- Erank K, Dennis S, Alison M, Tara K, Kevins S, et al. (2002) Variables associated with medication errors in pediatries emergency medicine. Pediatrics 110(4): 737-42.
- Howard AP (2003) Medication errors in the emergency department: a systems approach to minimizing risk. Emerg Med Clin North Am 21(1): 141-58.
- Marianne L, lars N and Jan Ma (2004) Errors in the medication process: m frequency, type, and potential clinical consequences. International journal for quality in health care Sept 27.
- Isah AO, Ross DD, Quick J, Laing R, Mabadeje AFB. The development of standard values for the WHO drug use prescribing indicators.
- Abdulahi M, Shiferaw T (1997) Pattern of prescription in Jimma Hosptial. Ethiop J Health Dev 11(3): 263–267.
- Desta Z, Abula T, Gebre YA, Worku A Drug prescribing patterns for outpatients in three hospitals in north-west Ethiopia. Ethiop J Health Dev 2002 16(2): 183-189.
- Assessment of the pharmaceutical sector in Ethiopia.
- WHO (1993) How to investigate drug use in health facilities: selected drug use indicators?
Article Type
Research Article
Publication history
Received Date: December 27, 2022
Published: February 15, 2022
Address for correspondence
Balisa Mosisa, School of Pharmacy, Institute of Health Sciences, Wollega University, Ethiopia
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Balisa M, Yeshi M, Lemessa B. Assessment of Medication Errors in Emergency Ward at Nekemte Referral Hospital, West Ethiopia. 2022- 4(1) OAJBS.ID.000398.
Table 1: Patient related information errors in NRH emergency ward (n=768) during, April, 2015.
Table 2: Prevalence of prescription errors and their distributions in NRH emergency department, April, 2015.
Table 3: Top ten antibiotic drugs prescribed in NRH at emergency department, April, 2015.
Table 4: Errors related with adequacy of drug storage in NHR at emergency ward, April, 2015.
Table 5: Errors related with adequacy of dispensary in NHR at emergency ward, April, 2015.