Analgesia for Total Knee Arthroplasty: A Randomized Controlled Study Comparing Local Infusion Analgesia, Femoral Nerve Block and Intrathecal Morphine
ABSTRACT
Introduction: The aim of this study was to compare the effectiveness of continuous intra-articular local infiltration analgesia,
femoral nerve block and intrathecal morphine for the management of post-operative pain and early function following total knee
arthroplasty.
Methods: A single center, three-armed parallel group, double blinded, randomized controlled pilot trial was undertaken. Patients
were randomized to receive either local infiltration analgesia, femoral nerve block or intrathecal morphine for post-operative
analgesia following total knee arthroplasty. The efficacy of analgesia was determined by recording post-operative pain visual
analogue scores, opiate requirements and side effects, and functional scores at 24 hours, 48 hours, and 6 weeks post-operatively.
Results: 45 patients were recruited to the study. 4 were excluded due to voluntary withdrawal and incomplete follow-up. The
final analysis included 13 patients randomized to the local infiltration analgesia group, 14 patients to the femoral nerve block
group and 14 patients to the intrathecal morphine group. There were no significant differences in post-operative pain scores, opiate
requirements and associated side effects, or functional scores at any point during the study period.
Conclusion: This study did not identify any significant differences between continuous intra-articular local infiltration analgesia,
femoral nerve block and intrathecal morphine for delivering post-operative an-algesia following total knee arthroplasty.
KEYWORDS
Knee; Arthroplasty; Analgesia; Local; Regional; Intrathecal
ABBREVIATIONS:
TKA: Total Knee Arthroplasty; LIA: Local Infusion Analgesia; FNB: Femoral Nerve Block; IM: Intrathecal Morphine; IV: Intravenous; TUG: Timed Up and Go (test); OKS: Oxford Knee Score; KSS: Knee Society Score; PRN: Pro Re Nata; PCA: Patient Controlled Analgesia; APS: Acute Pain Service; BMI: Body Mass Index
INTRODUCTION
An estimated 60% of patients report severe pain following total knee arthroplasty (TKA) [1]. Inadequate post-operative analgesia may be associated with poorer patient treatment satisfaction, longer hospital stays and increased costs [2,3]. High dose oral opiates carry risks of side effects such as nausea and vomiting, pruritus, reduced gut motility, sedation and respiratory depression. Therefore, a variety of techniques have been developed to deliver more effective post-operative analgesia such as local infiltration analgesia, peripheral nerve blockade, and intrathecal morphine. However, the relative analgesic efficacy of these techniques and their impact on post-operative opiate consumption and early mobility is unclear. Local infiltration analgesia via an infusion catheter has been shown to be more effective than single bolus administration, is easy to per-form and delivers analgesia directly to the source of pain [4]. However, there may be an increased risk of deep infection [5,6]. Femoral nerve blockade delivers analgesia away from the surgical site which, whilst not posing a risk of prosthetic joint infection, may not provide analgesia to the posterior joint. It may also reduce post-operative quadriceps power and ability for early mobilization, increasing the risk of falls [7]. Furthermore, it is technically more demanding, requires additional equipment, and is time consuming. In contrast intrathecal morphine may be delivered at the same time as spinal anesthesia and therefore the additional time required is negligible. One disadvantage, however, is the potential risk of opiate toxicity.
The aim of this study was to compare the efficacy of continuous intraarticular local anesthetic infusion, femoral nerve block and intrathecal morphine, for providing post-operative analgesia, reducing additional opiate consumption and associated side effects, and effect on early mobilization.
METHODS
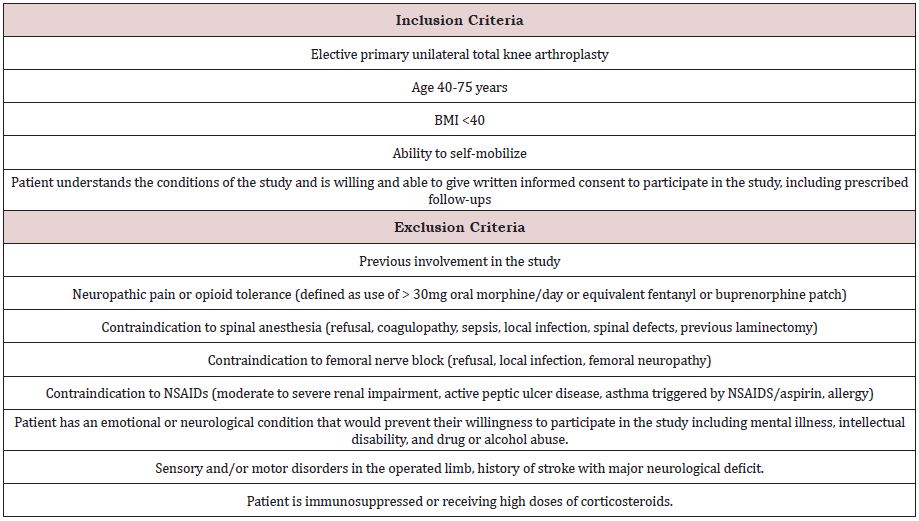
Three methods for delivering post-operative analgesia following total knee arthroplasty were compared in a single center, double blinded, randomized, place-controlled trial. An initial power calculation with 80% power and 5% significance indicated that a sample size of 59 patients in each group would be required. However due to limited funding a final cohort of 45 patients were recruited. Patients were randomized to receive either continuous intraarticular local infiltration analgesia (LIA), femoral nerve block (FNB) or intrathecal morphine (IM) using a randomization code generated with Excel software. All surgical procedures were performed at the Repatriation General Hospital, Adelaide, South Australia. The patient inclusion and exclusion criteria are given in Table 1.
Patients were identified for surgical eligibility from the waiting list for TKA and recruited and consented by a single research assistant. Anesthetic eligibility was confirmed by an Anesthetist during a pre-admission assessment one or two weeks before surgery.
All patients received 150mg pregabalin orally 1 hour preoperatively. The preparation of morphine, ropivacaine and placebo blinded products was undertaken by the hospital clinical trials pharmacy on the day before surgery. For spinal anesthesia the addition of morphine (200mcg morphine hydrochloride) or placebo (normal saline) to 2.5ml 0.5% bupivacaine was undertaken in the theatres immediately prior to intrathecal administration. Intrathecal anesthesia was delivered using a 25G Whitacre needle followed by an IV propofol infusion for sedation intra-operatively. Bolus femoral nerve injections were performed under ultrasound guidance and after administration of spinal anesthesia, using either 20ml 0.2% ropivacaine or placebo (20ml normal saline). All patients underwent standard total knee arthroplasty using a tourniquet and via medial parapatellar approach. 200ml of either 0.2% ropivacaine or placebo (normal saline) was delivered to the posterior capsule, medial, and lateral wound edges in roughly equal quantities at the end of the procedure. Immediately prior to closing an intra-articular wound infiltration catheter was inserted and connected to syringe driver to deliver 5ml 0.2% ropivacaine or placebo normal saline per hour for 24 hours, after which time the catheter was removed. Post-operatively all patients received 40mg IV parecoxib and 1g IV paracetamol. The patient group allocation and placebo materials were blinded to both the anesthetist and surgeon during the operation.
All patients were reviewed pre- and post-operatively (24 hours, 48 hours, 6 weeks) by a physio-therapist who collected data with regards to pain scores at rest and on walking, maximal knee flexion, distance covered in 2 minutes walking, and a ‘timed up and go test’ (TUG) defined as the time taken to stand from a seated position, walk a distance of 3 meters and return to the chair. Oxford Knee Scores (OKS) and Knee Society Score (KSS) were also recorded pre-operatively and at 6 weeks. All patients received routine postoperative oral analgesia of ibuprofen 400mg QDS and pregabalin 75mg BD. Additional analgesia was provided on a PRN basis of oxycodone 5mg-15mg hourly or fentanyl patient-controlled analgesia (PCA) as per the hospital protocol. The Acute Pain Service (APS) recorded and adjusted the use of oxycodone and fentanyl PCA at both 24 hours and 48 hours or prescribed additional tramadol in accordance with patient pain scores. Fentanyl PCA and tramadol use was converted to the equivalent oxycodone dose for postoperative opiate requirement comparisons between the groups. The presence of pruritus, nausea, vomiting, antiemetic use, hypotension requiring treatment, sedation or respiratory depression (RR<8, saturation <93%), requirement for urinary catheters, presence of a neurological block/deficit and blood transfusions was also recorded. Finally, the total length of hospital stay was recorded for each patient.
The results were compared between groups using ANOVA for continuous variables with post-hoc Tukey HSD tests as appropriate. Discrete data was analyzed using chi-squared tests. A p-value of less than 0.05 (two-tailed) was considered significant. All analyses were conducted using Excel (2010, Version 14.0.7214.5000).
RESULTS
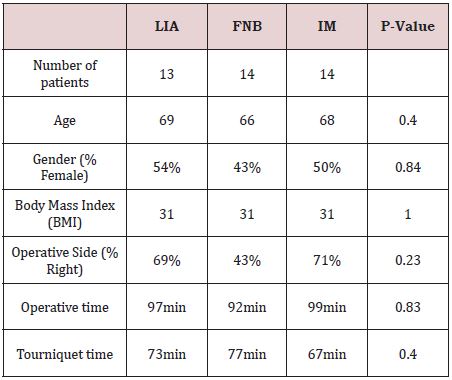
A total of 45 patients were recruited and randomized to one of the 3 treatment modalities. Four patients were not included in the final analysis due to voluntary withdrawal and incomplete followup, resulting in 13 patients randomized to the continuous intraarticular local infiltration analgesia (LIA) group, 14 patients to the femoral nerve block group (FNB) and 14 patients to the intrathecal morphine group (IM). The baseline demographics and operative treatment data is shown in Table 2. There were no significant differences between the groups in terms of age, gender, body mass index (BMI), operative side, operative time, or tourniquet time. No patients required post-operative blood transfusions.
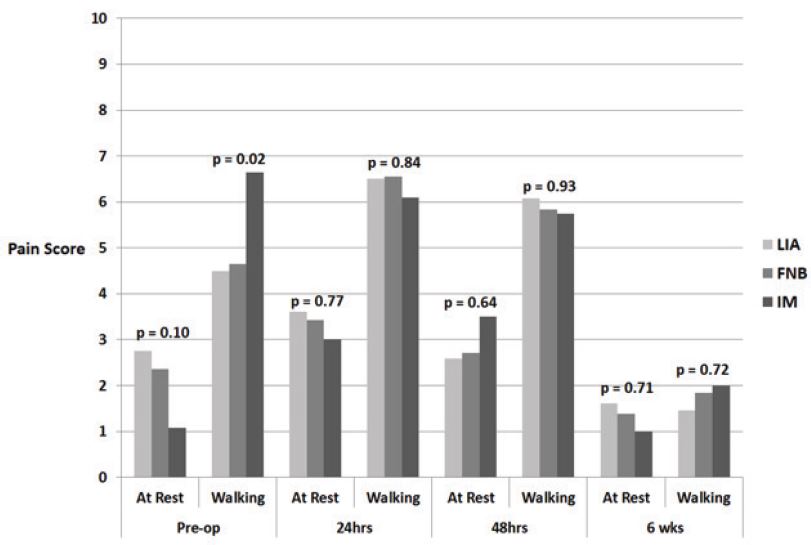
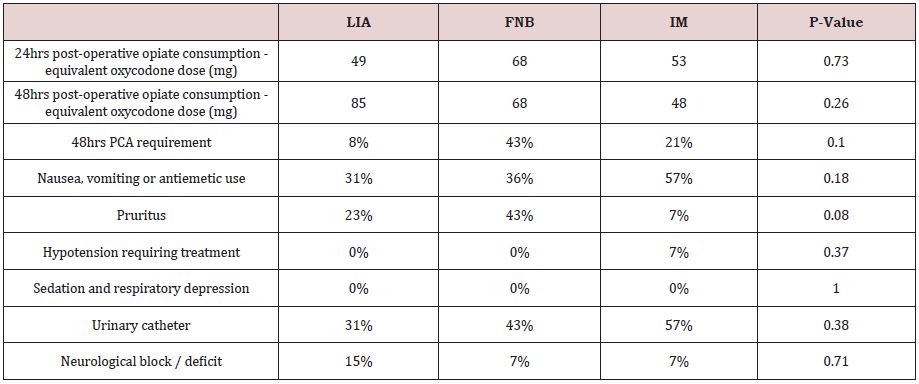
Pre-operative pain scores on walking were significantly greater in the IM group compared with the LIA group (ANOVA p=0.02, Tukey HSD p=0.04). However, there was no other difference in pain scores during follow-up between the groups, either at rest or with walking (Figure 1). In addition, there was no significant difference in post-operative opiate requirements in the first 24 hours or 48 hours between the groups. There was also no significant difference in the requirement for a PCA in the first 48 hours, or opiate side effects (Table 3).
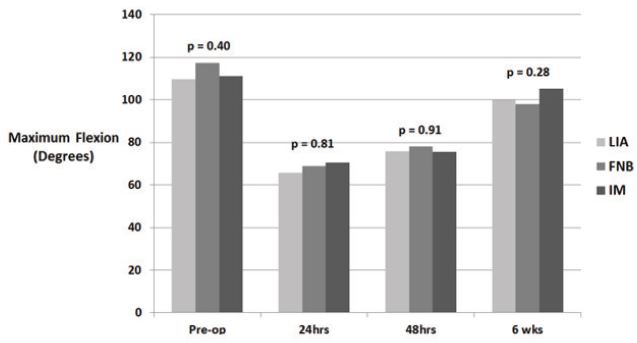
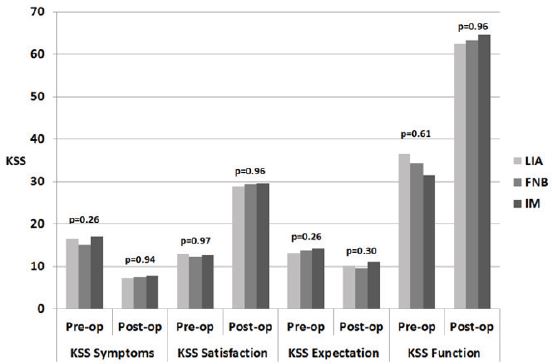
With regard to pre-operative function, there was no significant difference between patients’ base-line range of movement (Figure 2): flexion p=0.4, extension p=0.32), 2-minute walk test (p=0.84), TUG test (p=0.84) baseline OKS (p=0.83) or baseline KSS scores (Figure 3): symptoms p=0.26, satisfaction p=0.97, expectation p=0.26, function p=0.61) between the groups.
There was no significant difference in any of the follow-up time periods for degree of knee flexion (Figure 2), 2-minute walk tests (24 hours p=0.87, 48 hours p=0.27, 6 weeks p=0.09) or TUG tests (24 hours p=0.77, 48 hours p=0.70, 6 weeks p=0.44).
In addition, there was no significant difference in post-operative OKS (p=0.45) or KSS scores be-tween the groups (Figure 3). The mean length of stay was 5 days with no significant difference between the groups (p=0.45).
DISCUSSION
The results of this study do not demonstrate any significant differences between local infiltration analgesia, femoral nerve block or intrathecal morphine for providing post-operative analgesia or reducing additional opiate consumption and side effects. In addition, there were no differences in post-operative rehabilitation.
The results of other studies investigating the analgesia effects of these techniques have produced conflicting results. Comparing LIA with placebo, Williams et al did not demonstrate any significant benefit of a continuous intra-articular bupivacaine infusion compared with placebo for reducing pain scores, opiate consumption, opioid side effects, length of stay or knee function [8]. In contrast, Ali et al identified lower pain scores in the first post-operative day with a continuous ropivacaine infusion versus placebo [5]. However, there was no difference in additional opiate consumption, knee function or length of stay. A meta-analysis by Zhang et al. [9] analyzing seven studies com-paring LIA with placebo also concluded that LIA appeared to offer better postoperative analgesia. However, there are concerns that LIA may be associated with an increased risk of deep infection, possibly relating to colonization of the infusion catheter.
Comparing LIA with FNB, Mei et al. [10] demonstrated lower pain scores with FNB upon movement but otherwise no significant differences in pain scores at rest, or opioid consumption at 24hours were identified. In contrast, Yun et al demonstrated better pain scores at 6 hours post-operatively with LIA when compared with FNB, although this effect was not sustained at 24 hours [11]. Antoni et al. [12]; Stathellis et al. [13] both demonstrated better post-operative analgesia with LIA when compared with FNB, with quicker rehabilitation and shorter hospital stay. Zinkus et al. [14] did not demonstrate any difference in analgesic effects between LIA and FNB. However, they identified reduced opiate consumption and improved knee function with LIA at 1 week and 1 month postoperatively. Interestingly, a study by Reinhardt et al. [15] comparing LIA with a combination of FNB and IM, concluded that LIA was less effective for providing post-operative analgesia but improved rehabilitation probably due to retained quadriceps strength. Chang et al. [16]; Kunopart et al. [17] have also demonstrated that combining IM with FNB improves post-operative analgesia and reduces additional opiate consumption, highlighting the benefit of utilizing a multi-modal approach.
Several studies have also compared FNB with IM. Olive et al demonstrated an inferior analgesic effect and poorer mobility with IM compared with FNB, with more patients reporting pruritus [18]. In contrast studies by Sundarathiti et al. [19]; Tarkkila et al. [20]; Frassanito et al. [21] identified better pain control with IM over FNB, although opiate side effects were again more prevalent in the IM group. In a study by Sites et al there was no difference in analgesic effect or additional opiate consumption between IM and FNB [22]. However, the increased risk of opiate side effects with IM resulted in poor patient treatment satisfaction.
A greater risk of opiate side effects with IM have also been shown in studies comparing IM with LIA. Tammachote et al. [23] did not demonstrate any significant difference in analgesia effect between LIA and IM but more patients in the IM group complained of nausea, vomiting and pruritus. Similarly, a meta-analysis by Jia et al identified that LIA appeared to provide superior analgesia with fewer side effects [24]. Essving et al. [25] also compared LIA with IM and identified that LIA pro-vided better analgesia, reduced additional opiate consumption and facilitated quicker recovery with shorter length of stay and better patient satisfaction compared with IM. However, they did not notice any difference in opiate side effects.
This study has several limitations. Firstly, due to the limited funding available and recruitment, this study may be underpowered. Nonetheless we believe the methodology of this study to be robust, with placebo controls and blinding as strengths to reduce the risk of bias. It is also important to recognize that significant variation exists in clinical practice regarding the types of local anesthetics used, their dosage, additional drug combinations, delivery sites and techniques. In this study a low dose femoral nerve block was selected to minimize the effect on motor function and post-operative mobilization. However other techniques, such as adductor canal blocks are also be-coming popular due to their minimal motor blockade. As a result, it is not possible to investigate every possible approach. Furthermore, a multi-modal approach to delivering postoperative analgesia may be more important and effective than relying on any one individual technique, by capitalizing on multiple mechanisms of action and enabling the use of lower doses to reduce potential side effects.
CONCLUSION
This study did not identify any significant differences between local infiltration analgesia, femoral nerve block and intrathecal morphine for delivering post-operative analgesia following total knee arthroplasty. We therefore recommend that the technique of analgesia employed be based on surgeon preference and tailored to individual patients in light of their suitability for spinal anesthesia, estimated tolerance to rehabilitation regimens, infection risk and past susceptibility to opiate side effects.
TRIAL REGISTRATION NUMBER
ID ACTRN12613000983707. The study was registered with the Australian New Zealand Clinical Trials Registry.
REFERENCES
- Singelyn FJ, Deyaert M, Joris D (1998) Effects of intravenous patientcontrolled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg 87(1): 88-92.
- Barrington JW, Halaszynski TM, Sinatra RS (2014) Perioperative pain management in hip and knee replacement surgery. Am J Orthop 43(4): S1-S16.
- Hamilton TW, Strickland LH, Pandit HG (2016) A meta-analysis on the use of gabapentinoids for the treatment of acute postoperative pain following total knee arthroplasty. J Bone Joint Surg Am 98(16): 1340- 1350.
- Zhang S, Wang F, Lu ZD (2011) Effect of single-injection versus continuous local infiltration analgesia after total knee arthroplasty: a randomized, double-blind, place-controlled study. J Int Med Res 39(4): 1369-1380.
- Ali A, Sundberg M, Hansson U (2015) Doubtful effect of continuous intraarticular analgesia after total knee arthroplasty: a randomized double-blind study of 200 patients. Acta Orthop 86(3): 373-377.
- Sun XL, Zhao ZH, Ma JX, Li FB, Li YJ, et al. (2015) Continuous local infiltration analgesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 94(45): e2005.
- Sharma S, Iorio R, Specht L, Davies-Lepie S, Healy W (2010) Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res 468(1): 135-140.
- Williams D, Petruccelli D, Paul J (2013) Continuous infusion of bupivacaine following total knee arthroplasty: a randomized control trial pilot study. J Arthroplasty 28(3): 479-484.
- Zhang Y, Lu M, Chang C (2017) Local anesthetic infusion pump for pain management following total knee arthroplasty: a meta-analysis. BMC Musculoskelet Disord 18(1): 32.
- Mei S, Jin S, Chen Z, Ding X, Zhao X, et al. (2015) Analgesia for total knee arthroplasty: a meta-analysis comparing local infiltration and femoral nerve block. Clinics 70(9): 648-653.
- Yun XD, Yin XL, Jiang J, Teng YJ, Dong HT, et al. (2015) Local infiltration analgesia versus femoral nerve block in total knee arthroplasty: a metaanalysis. Orthop Traumatol Surg Res 101(5): 565-569.
- Antoni M, Jenny JY, Noll E (2014) Postoperative pain control by intraarticular local anesthesia versus femoral nerve block following total knee arthroplasty: impact on discharge. Orthop Traumatol Surg Res 100(3): 313-316.
- Stathellis A, Fitz W, Schnurr C, Koeck FX, Gebauer M, et al. (2017) Periarticular injections with continuous perfusion of local anaesthetics provide better pain relief and better function compared to femoral and sciatic blocks after TKA: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc 25(9): 2702-2707.
- Zinkus J, Mockutė L, Gelmanas A, Tamošiūnas R, Vertelis A, et al. (2017) Comparison of 2 analgesia modalities in total knee replacement surgery: is there an effect on knee function rehabilitation? Med Sci Monit 23: 3019-3025.
- Reinhardt KR, Duggal S, Umunna BP, Reinhardt GA, Nam D, et al. (2014) Intraarticular analgesia versus epidural plus femoral nerve block after TKA: a randomized, double-blind trial. Clin Orthop Relat Res 472(5): 1400-1408.
- Chang KP, Choon KC, Hyun HS, Jung HC (2008) The effect of intrathecal morphine added to continuous femoral 3-in-1 nerve block for analgesia after total knee replacement. Korean Journal of Anesthesiology 54: 544- 551.
- Kunopart M, Chanthong P, Thongpolswat N, Intiyanaravut T, Pethuahong C (2014) Effects of single shot femoral nerve block combined with intrathecal morphine for postoperative analgesia: a randomized, controlled, dose-ranging study after total knee arthroplasty. J Med Assoc Thai 97(2): 195-202.
- Olive DJ, Barrington MJ, Simone SA, Kluger R (2015) A randomised controlled trial comparing three analgesia regimens following total knee joint replacement: continuous femoral nerve block, intrathecal morphine or both. Anaesth Intensive Care 43: 454-460.
- Sundarathiti P, Thammasakulsiri J, Supboon S, Sakdanuwatwong S, Piangjai M (2016) Comparison of continuous femoral nerve block (CFNB/SA) and continuous femoral nerve block with mini-dose spinal morphine (CFNB/SAMO) for postoperative analgesia after total knee arthroplasty (TKA): a randomized controlled study. BMC Anesthesiol 16(1): 38.
- Tarkkila P, Tuominen M, Huhtala J, Lindgren L (1998) Comparison of intrathecal morphine and continuous femoral 3-in-1 block for pain after major knee surgery under spinal anesthesia. Eur J Anaesthesiol 15(1): 6-9.
- Frassanito L, Vergari A, Zanghi F, Messina A, Bitondo M, et al. (2010) Post-operative analgesia following total knee arthroplasty: comparison of low-dose intrathecal morphine and single-shot ultrasound-guided femoral nerve block: a randomized, single blinded, controlled study. Eur Rev Med Pharmacol Sci 14(7): 589-596.
- Sites BD, Beach M, Gallagher JD, Jarrett RA, Sparks MB, et al. (2004) A single injection ultrasound-assisted femoral nerve block provides side effect-sparing analgesia when compared with intrathecal morphine in patients undergoing total knee arthroplasty. Anesth Analg 99(5): 1539- 1543.
- Tammachote N, Kanitnate S, Manuwong S, Yakumpor T, Panichkul P (2013) Is pain after TKA better with periarticular injection or intrathecal morphine? Clin Orthop Relat Res 471(6): 1992-1999.
- Jia XF, Ji Y, Huang GP, Zhou Y, Long M (2017) Comparison of intrathecal and local infiltration analgesia by morphine for pain management in total knee and hip arthroplasty: A meta-analysis of randomized controlled trial. Int J Surg 40: 97-108.
- Essving P, Axelsson K, Åberg E, Spännar H, Gupta A, et al. (2011) Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg 113(4): 926-933.
Article Type
Research Article
Publication history
Received Date: January 25, 2022
Published: February 23, 2022
Address for correspondence
Christopher Wilson, Department of Orthopaedics, University of Flinders and Flinders Medical Centre, Australia
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Johnathan D C, Jason G K, Jeganath K, Christopher J W. Analgesia for Total Knee Arthroplasty: A Randomized Controlled Study Comparing Local Infusion Analgesia, Femoral Nerve Block and Intrathecal Morphine. 2022- 4(1) OAJBS.ID.000403.
Figure 1: Mean pain scores for LIA, FNB and IM, at rest and walking, pre-operatively and at 24 hours, 48 hours and 6 weeks post-operatively.
Figure 2: Maximum knee flexion pre-operatively and at 24 hours, 48 hours and 6 weeks post-operatively.
Figure 3: KSS scores pre-operatively and 6 weeks post-operatively.
Table 1: Study inclusion and exclusion criteria.
Table 2: Baseline demographics.
Table 3: Opiate consumption and side effects.