A Review of Iodine Nutrition Situation in Bhutan; Historical Milestones
ABSTRACT
Iodine is a micronutrient required for production of thyroid hormones which plays a critical role in metabolism. Iodine
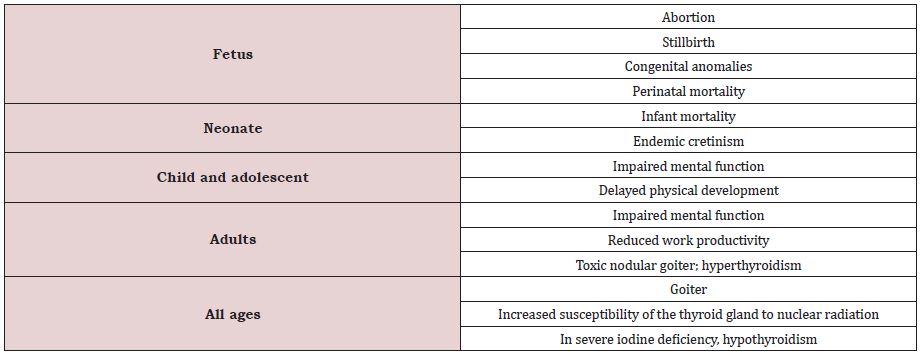
deficiency can lead to many severe effects throughout the human life cycle and is collectively termed as iodine deficiency disorders.
Salt fortification is an effective intervention to improve iodine nutrition in the population. In Bhutan, iodine deficiency disorders
(IDD) were universally present with the first nationwide survey conducted in 1983, reporting a total goiter rate of 64.5%. This lead
to establishment of ‘Nutrition Section’ in the Directorate of Health and the Iodine Deficiency Disorders Control Program (IDDCP) in
planning commission in 1985.
Several public health interventions were undertaken to address this public health burden; salt iodization and distribution, iodized
oil injections, establishment of the Bhutan Salt Enterprise in Phuntsholing and program evaluation. Since then, many assessments
were conducted to evaluate the program all of which reported significant improvements. In 2003 an external monitoring team
confirmed that Bhutan was the first country in WHO SEARO to have eliminated IDD as a public health problem.
An assessment conducted in 2010 reported that Bhutan was sustaining the IDD elimination status achieved in 2003. Constant
program improvements and investments are required to sustain this achievement. Iodine content of various salt brands needs to be
analyzed from time to time to regulate import control and surveys must be conducted periodically for program evaluation.
KEYWORDS
Bhutan; Iodine; Deficiency; Historical milestones; Elimination
INTRODUCTION
Iodine is a natural chemical element of the earth occurring in various forms such as Iodide (I), Iodate (IO3) and elemental Iodine (I2) [1]. Iodine is required for production of thyroid hormones thyroxine (T4) and triiodothyronine (T3) [2]. Thyroid hormones play a critical role in metabolism (2) and deficiency of iodine can lead to many adverse effects throughout the human life cycle which is collectively termed as iodine deficiency disorders (IDD) [3]. Globally around two billion people suffer iodine deficiency of which around 50 million present clinical manifestations [4].
The World Health Organization (WHO) reports that iodine deficiency is the single most important cause of preventable brain damage [5]. Swelling of thyroid gland, termed as goiter is the most visible effect of iodine deficiency, but the most serious is cognitive impairment as thyroid hormones are required for ‘neocorticogenesis’, an early process in development of the central nervous system in fetus [6]. People living in areas affected by severe iodine deficiency may have their intelligence quotient (IQ) reduced by 13.5 points and these deficiencies have an immediate effect on child learning capacity and economic productivity [5];(Table 1).
SOURCES AND DIETARY REQUIREMENT
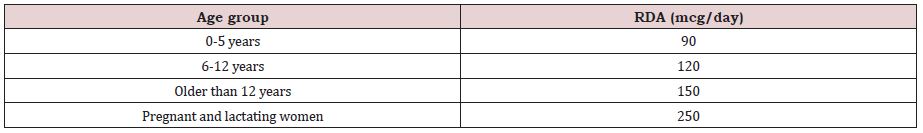
Iodine is widely but unevenly distributed in the earth’s environment in iodide form. Leaching and soil erosion leads to depletion of iodide from surface soil and most of iodide is found in the ocean [7]. Foods of marine origin usually have a higher iodine content due to higher concentration of iodine in seawater; however, iodized salt is the major source of iodine. Adding iodine to salt is considered as one of the most efficient ways to improve iodine nutrition. The WHO recommends fortification of salt with 20-40mg of iodine per kilogram of salt, which can be added either as potassium iodide or potassium iodate(7). The recommended daily allowance (RDA) of iodine varies by age group [7] which is described in the Table 2 below.
Historical Evidence of Iodine Deficiency Disorders in Bhutan
The earliest evidence of iodine deficiency disorders in Bhutan dates back to 1873 when surgeon Robert Saunders travelled on a mission from India to Tibet through Bhutan. Saunders, who is also referred to as path breaking in terms of Goiter reported that “Of the diseases in this country, the first that attracts our notice as we approach the foot of the hills, is a glandular swelling of the throat”. Despite the disease being very common with one in six people effected, it was accorded very little attention [8].
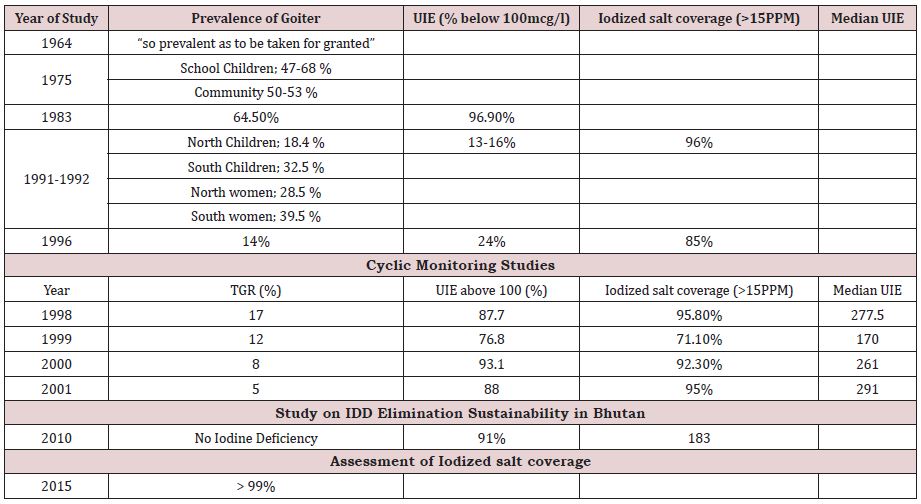
Iodine deficiency disorders was recognized as a major public health problem in Bhutan since the 1960’s [9]. The first known published report on IDD in Bhutan was by two English doctors in 1964. During their five-week observational study, they reported that goiter was “so prevalent as to be taken for granted” [10]. Considering the severity of the situation, the Government initiated the importation of iodized salt from India. However, this was discontinued in 1970 because of poor acceptance by the population due to bad appearance and flavor. A study conducted in 1975 in nine districts reported a goiter prevalence rate of 47-68% in school children and 50-53% in adult population.
Past IDD Studies and Historical Milestones
The first nationwide IDD survey conducted in 1983 reported total goiter rate at 64.5%, cretinism around 10% and low urine iodine concentration in majority of the population [9,10]. To address this huge public health problem, ‘Nutrition Section’ was established under the Directorate of Health Services and ‘Nutrition Cell’ was created for a coordinated multi-sectoral Iodine Deficiency Disorders Control Program (IDDCP) under the Planning Commission in 1985. The major components of IDDCP were salt iodization and distribution, iodized oil injections, monitoring of iodine in salt and program evaluation. Subsequently a salt iodization plant named Bhutan Salt Enterprise (BSE) was commissioned in Phuentsholing in April 1985. The plant had capacity of 6 tons per hour and produced iodized salt at 60 parts per million (PPM) using standard continuous spray mixing technique. The Government controlled importation and distribution of salt and regulations were in place to prevent import of salt not routed through salt iodization plant.
As a short-term measure, iodized oil injections were administered to women of childbearing age in the southern boarder districts from 1988 and the campaign was completed in 1991. The Nutrition cell was handed over to the Nutrition section in 1990 and currently the Nutrition Program, Department of Public Health, Ministry of Health manages the IDDCP [9].
A second nationwide study was conducted between 1991 and 1992 to assess the impact of IDDCP. The study found that total goiter rate was 18.4% among children in northern region and 32.5% in southern region. The prevalence of cretinism was 0.4% in children in both the regions. Goiter prevalence among women in the north was 28.5% and 49.5% among women in the south. Cretinism was 0.9% and 0.8% among women in north and south respectively. The median urine iodine excretion (UIE) was 283mcg/l and 244mcg/l among children in the north and south respectively. The study also found that 96.6% of the households in the north and 95.0% of the households in the south had acceptable iodine level in salt (more than 15 PPM) [9].
A third study was titled ‘tracking progress towards sustainable elimination of iodine deficiency disorders in Bhutan’ was conducted in 1996. The study found that 74% of the salt samples had adequate levels of iodine (>25ppm) at retail level and 82% of the salt samples had adequate level of iodine (>15ppm) at household level. The median urine iodine excretion was 230mcg/l but 24% of the urine samples had UID less that 100mcg/l and total goiter rate (TGR) at 14%. Bhutan was then classified as ‘MILD’ iodine deficiency country. The study recommended introducing cyclic monitoring of IDDCP covering every district in five years.
On 30th August 1997, His Holiness the Je Khenpo (Chief Abbot of the central monastic body of Bhutan) issued a decree on consumption of iodization salt [11]. The decree describes the importance of iodine for optimal growth and cognitive development (Table 3).
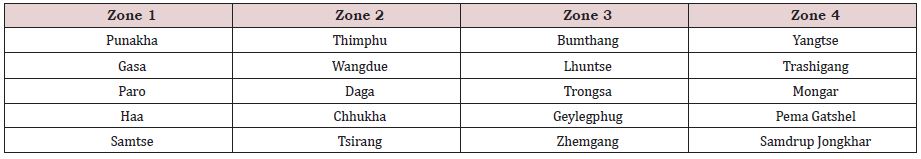
Cyclic monitoring was initiated in 1998 by grouping the country into four zones covering a zone every year. Monitoring was conducted by randomly selecting 30 clusters from each zone. 40 school children between 6-11 years were randomly selected and examined for goiter from each cluster. Urine and salt samples were also collected from every 4th student [12]. A citation handed over to the Government of Bhutan states that “Bhutan maybe one of the first countries in the world to have begun annual cyclic monitoring in addition to the regular monitoring system” [10] (Table 4).
The cyclic monitoring studies found that median UIE was above 200mcg/l. Recommendations were made to reduce salt iodization at production level from 60ppm to 50ppm [13]. In August 2002, the government approved five recommendations on salt iodization.
The key recommendations were adopting Codex standard for salt quality, establishing a salt testing laboratory, testing of salts for heavy metal contamination and banning the import of any brand of salt if it does not meet the quality standard [14].
Current IDD Status in the Country
An external evaluation team assessed and confirmed that Bhutan had achieved all the 10-point programmatic indicators set by the WHO for sustainable elimination of IDD [13]. The WHO considers attainment of 8 out of 10 programmatic indicators in addition to iodized salt coverage of over 90% and median urine excretion over 100μg/L in the general population as sustainable elimination IDD as a public health problem [15]. The team declared Bhutan as the first country in WHO SEARO to have eliminated IDD as a public health problem [13].
In September 2003, WHO, UNICEF and IDD Consortium jointly certified that Bhutan has moved from severe iodine deficiency to ‘Adequate Iodine Nutrition’ status. Further they stated that “Bhutan is an excellent example of how the nutrition welfare of a nation can be significantly improved by commitment and hard work” [15].
In 2010 a study was conducted in children aged 6-11 years to evaluate the sustenance of elimination of Iodine Deficiency Disorders in Bhutan. The study found that the 91% of the salt samples had adequate iodine content and the national median urine iodine excretion was 183μg/L. According to the World Health Organization, urine iodine excretion equal to or greater than 100μg/L is indicative of optimal iodine nutrition. Regional and district wise analysis of the same study found that Tashigang and Samdrup Jongkhar districts in eastern Bhutan had median urine excretion of 88μg/L and 69μg/L respectively, indicating a mild iodine deficiency and recommended that monitoring be strengthened in these two districts.
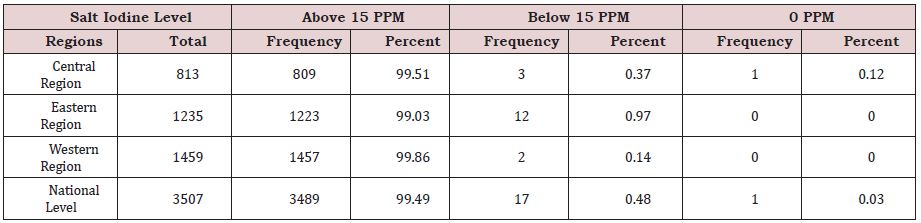
In 2015, during the conduct of a nationally representative Nutrition Survey, salt samples were collected from all households and analyzed qualitatively using rapid test kit. The assessment found that iodized salt coverage was over 99% [16]. However, urine iodine excretion and iodine level in salt was not studied. The data was maintained with the Nutrition program and is being published for the first time (Table 5).
Current Salt Monitoring System
Phuentsholing Hospital and Bhutan Agriculture and Food Regulatory Authority (BAFRA) monitor salt iodine levels at production level at the Bhutan Salt Enterprise [17]. At the wholesale and retail level monitoring is conducted by BAFRA and district hospital. Local health staff conduct monitoring at household level on a monthly basis. Ten random samples are collected every month from catchment areas of respective health facility and tested using rapid test kit. Any doubtful samples are shipped to Royal Centre for Disease Control (RCDC) for confirmatory test conducted using titration method. Any salt sample that does not meet the required iodization level is advised to discard and people are advised not to buy that particular brand of salt. A web-based salt iodine monitoring system (SIMS) was developed and implemented in 2018 to strengthen the salt monitoring system and guideline to sustain the IDD elimination status was revised in 2021 [16].
CONCLUSION AND RECOMMENDATIONS
Bhutan has been successful in eliminating iodine deficiency disorders as a public health problem since 2003. However, several recommendations including constant surveillance needs has to be implemented to sustain this achievement. There is a need for periodic assessments to evaluate the program and generate recommendations. Analysis of various salt brands also needs to be conducted from time to time to have evidence informed import control and salt monitoring system needs to be strengthened. Advocacies and exercises must be conducted to synchronize salt reduction and salt iodization strategies. There is a need to define clear roles and responsibilities of different monitoring bodies and sensitize policy makers to keep them updated on IDDCP to keep the iodine nutrition as a national priority.
REFERENCES
- Iodine Global Network. What is iodine.
- National Institutes of Health, Office of Dietary Supplements. Iodine Fact Sheet for health professionals (2021).
- Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine deficiency disorders. Lancet 372: 1251-1262.
- Lazarus JH (2015) The importance of iodine in public health. Environ Geochem Health 37(4): 605-618.
- WHO (2007) Assessment of iodine deficiency disorders and monitoring their elimination.
- Auso E, Lavado AR, Cuevas E, Rey F, Escobar G, et al. (2004) A Moderate and transient deficiency of maternal thyroid function at the beginning of fetal neocorticogenesis alters neuronal migration. Endocrinology 145(9): 4037-4047.
- Iodine Global Network. Where do we get Iodine from?
- Valancius L, Lipscombe T (2020) Healing in the Himalayas: Robert Saunders, surgeon, and the embassy to Bhutan and Tibet of 1783. Journal of Bhutan Studies 42.
- (1996) Nutrition Section, Directorate of Health Services, Royal Government of Bhutan. Tracking Progress towards Sustainable Elimination of Iodine Deficiency Disorders (IDD) in Bhutan./li>
- AIIMS. Citation to Royal Government of Bhutan for pioneering efforts towards sustaining elimination of Iodine Deficiency Disorders in Bhutan.
- (1997) Decree by His Holiness the Je Khenpo. Kuensel.
- (2002) Nutrition Section, Directorate of Health Services. Internal Evaluation of IDCCP by cyclic monitoring.
- (2007) Ministry of Health, Royal Government of Bhutan, UNICEF, WHO, ICCIDD, AIIMS, BSE. Tracking progress towards sustaining elimination of iodine deficiency disorders in Bhutan.
- (2002) Ministry of Agriculture and Forests. Royal Government of Bhutan. Government recommendations on iodized salt.
- (2003) WHO, UNICEF. Adequate Iodine Nutrition status in Bhutan.
- (2015) Nutrition Program, Ministry of Health. Royal Government of Bhutan.
- (2010) Nutrition Program and Public Health Laboratory. Operational Guideline on Sustaining Iodine Deficiency Disorder Elimination in Bhutan. 2nd edn. Thimphu.
Article Type
Review Article
Publication history
Received Date: December 12, 2021
Published: January 04, 2022
Address for correspondence
Hari Prasad Pokhrel, Department of Public Health, Ministry of Health, Bhutan
Copyright
©2022 Open Access Journal of Biomedical Science, All rights reserved. No part of this content may be reproduced or transmitted in any form or by any means as per the standard guidelines of fair use. Open Access Journal of Biomedical Science is licensed under a Creative Commons Attribution 4.0 International License
How to cite this article
Hari PP, Laigden D, Vishal C, Tandin D. A Review of Iodine Nutrition Situation in Bhutan; Historical Milestones. 2022- 4(1) OAJBS.ID.000371.